Download PDF
Abstract
Background
By streamlining workflows at the point of care and enabling secure real-time and rapid transfer of patient data across the healthcare delivery organization (HDO) network, mobile devices offer opportunities to increase clinician workflow efficiency, user satisfaction, teamwork and communication. However, accompanying the benefits of clinical mobility are concerns related to data privacy, security, and proper authentication, which can make it difficult to efficiently manage shared mobile devices as they are exchanged between clinical users. Measures that enhance security can often impede usability and adoption, such that HDOs may struggle to optimize their investments in mobile technology. In this study, the authors gathered information regarding the perceptions in US HDOs on the perceived value, utilization, and management challenges of a clinical mobile devices fleet.
Methods
An anonymous, online survey was deployed to eligible respondents assessing HDO mobile devices use level, applications accessed, impact on users when lost, and related organizational challenges.
Results
Almost half (97; 47.5%) of the 204 survey respondents regarded mobile devices as conveying greater efficiency than workstations for completing clinical work. A majority (126; 61.7%) deployed 500 or fewer mobile devices and 48.3% (98) estimated that 2-4 applications were accessed per shift; 33.7% (69) accessed 5-14 applications. Clinical communications (141; 69.2%) and the electronic health record (EHR) (136; 66.7%) were most frequently accessed. Two-thirds of respondents (133; 65.1%) estimated applications were accessed more than 10 times per shift. Half reported that a lost device delays patient care. Only 37.2% (76) desired greater mobile device deployment in the future, with 41.9% undecided.
Conclusions
Mobile workflows are becoming integral to the healthcare information ecological system, enabling bedside access to the EHR and clinical applications. HDOs seek the benefits mobility can add to care delivery and clinician experience, but perceive managing an enterprise mobile device fleet as complex and challenging. Mobile access management tools are needed to streamline rapid, secure device authentication and information access with improved interoperability, user experience, and workflow flexibility while reducing the IT administrative burden of mobile device fleet management.
INTRODUCTION
Device mobility in healthcare delivery organizations (HDOs) is transforming point-of-care workflows, making them simpler and more streamlined. Shared-use mobile devices – smartphones or tablets that are enterprise owned and shared among clinicians – offer user increased flexibility and cost savings over bring your own device (BYOD) strategies.1,2 The number of Internet of Medical Things (IoMT) devices is expanding rapidly; the synergies with mobility in healthcare are also driving mobile device deployment.3 Mobile devices streamline workflows at the point of care by enabling real time and secure access to patient data, which can demonstrably increase clinical workflow efficiency, improve team communication and collaboration, and enhance satisfaction among both clinicians and patients.4–6 Clinical workflows at the bedsid,e which utilize mobile device technology, have resulted from growing device interoperability.7,8
Mobile solutions increase workflow flexibility by facilitating easier care team communication and collaboration; they can potentially improve HDO financial performance and human resource management.3 In addition, the cost, management, and maintenance of a mobile device fleet is considerably less resource-intensive than traditional computer workstations; mobile devices also have a large and expanding number of useful clinical applications.7,9 Given these capabilities and value, clinician use of mobile devices is projected to continue increasing.6,7
Clinical mobility brings with it challenges in ensuring data privacy, security, and access with proper authentication, which are made more complex by shared-use mobile devices that are exchanged among clinicians.10–12 Mobile devices can be implemented without diminishing security or privacy; however, this requires a dedicated enterprise effort.9,11,12 Measures implemented to ensure cybersecurity can nonetheless decrease the usability of mobile technology.8,9 Effective management of digital identity is central to HDO effectiveness in maintaining security while minimizing both risks of mobile device exposure and usability barriers.
This study shares the findings of a US survey of HDO leaders and mobile device using clinicians that collected information about their viewpoints and experiences relating to hospital/system imperatives and unmet needs in managing (and maximizing the value of) a mobile device fleet. It deepens and expands the focus of a prior multinational report across four nations on how mobile devices are being utilized in care delivery and the associated challenges in managing an enterprise-owned shared device (EOSD) mobile strategy.12
METHODS
Study Design
An online survey using the SurveyMonkey (Palo Alto, CA) Audience Targeting solution was deployed to eligible respondents working in a variety of clinical and information technology roles impacted by increasing use of mobile devices in HDOs. This study did not involve patients or patient data, and the survey of healthcare personnel and mobile device users was completed on an opt-in basis where respondents explicitly consented to have their data published in aggregate, deidentified form. As such, IRB approval was not required.
Respondent Selection and Characteristics
Mobile device clinical users, other staff, and information technology (IT) services managers within HDOs were identified exclusively through the SurveyMonkey Audience Targeting solution, sampling respondents from health systems, hospitals, and other clinical care delivery settings who had previously joined the SurveyMonkey Contribute Panel. Potential respondents were sent an email invitation to participate in the survey. Eligibility criteria for survey participation included being a current or potential active user of EOSD devices and contributing to organizational decisions regarding the management of mobile device functionality, access and distribution at their respective organizations. Targeting criteria within the Survey Monkey national survey respondent pool were also developed. Participant selection criteria included the following: 25-65 years with basic census balancing; both genders with no gender balancing; working within the US in any/all regions with no regional balancing; industry specified as healthcare with job functions of physician, nurse, healthcare provider (other than physician or nurse).
Survey Development and Distribution
The 19-question, anonymous survey (Supplemental Material) was created in SurveyMonkey (Palo Alto, CA) and distributed exclusively via email. The survey was implemented and completed on a single day, October 31, 2023, and survey responses were analyzed and tabulated in December and January 2024. The target number of surveys were completed on the first day, and no subsequent email reminders were required. The survey content and question items were developed and pre-tested by individuals working at Imprivata (Waltham, MA). Participants were not compensated, but a 50-cent contribution was made by SurveyMonkey to the charity of the respondent’s choice for completing the survey.
Survey questions gathered information about respondents’ organizational role(s), clinical care setting in which they worked, quantity of HDO mobile devices, use level or frequency of mobile device use, whether mobile devices were shared and enterprise-owned or bring your own device (BYOD), nature and estimated number of applications accessed through mobile devices per shift, frequency of users forgetting mobile device passwords, impact on users when their mobile device is missing or misplaced, and perceived organizational benefits of greater mobile device use.
Data Analysis
Survey data was analyzed using stratified contingency figures, evaluating key variables and responses of greatest pertinence to understanding the current status of and gaps, concerns, needs and challenges in mobile device use and management.
RESULTS
Respondents
The total sample size of completed surveys was 204, with a survey completion rate of 60% of the total survey pool. The survey response denominator varied by question, ranging from 120-204. In terms of professional role, 47.1% (96) of respondents were allied health professionals (including physical, occupational, or respiratory therapists), 36.3% (74) were nurses or nurse practitioners, 9.8% (20) were physicians or physician assistants, 4.4% (nine) were laboratory technicians. Together, allied health and nursing professionals comprised 83.4% (170) of respondents. The remaining respondents were in other roles such as information technology management, patient transport, or environmental services.
Respondents were located in large coastal cities and major urban areas: 48 were located in the mid-Atlantic and southeast US; 36 were in the mid-west central US; 30 in the mid-Atlantic and 26 in the Pacific region; and 26 in the Pacific region. Most respondents worked in an outpatient care setting (58; 28.7%) or in home health/skilled nursing or a behavioral health facility (57; 28.2%). Others worked in either a large (500+ beds, 44; 21.5%) or small (<500 beds, 44; 21.5%) independent delivery network (IDN).
Device Trends
Most (120; 58.7%) respondents indicated that their HDOs used EOSDs rather than a bring-your-own device model.
With respect to number of mobile devices deployed, 61.7% (126) reported having 500 or fewer mobile devices facility or enterprise wide. A further 17.5% (36) reported having 500-1000 mobile devices, and 20.8% (42) had greater than 1000 mobile devices deployed (Figure 1). Figure 2 shows the number of devices by care setting; as one might expect, respondents from larger hospitals and IDNs reported greater numbers of mobile devices deployed.
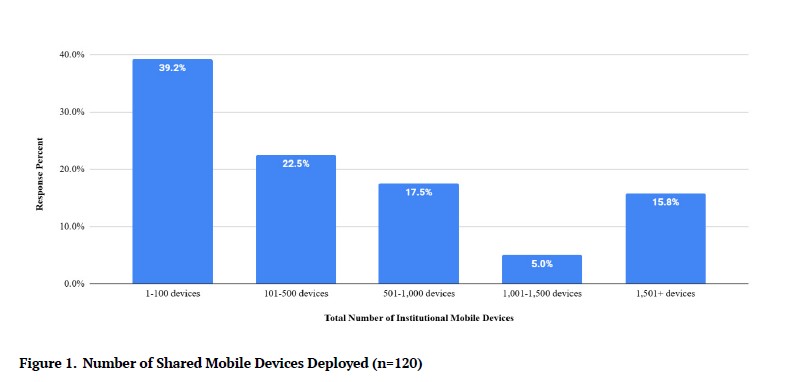
Figure 1.Number of Shared Mobile Devices Deployed (n=120)
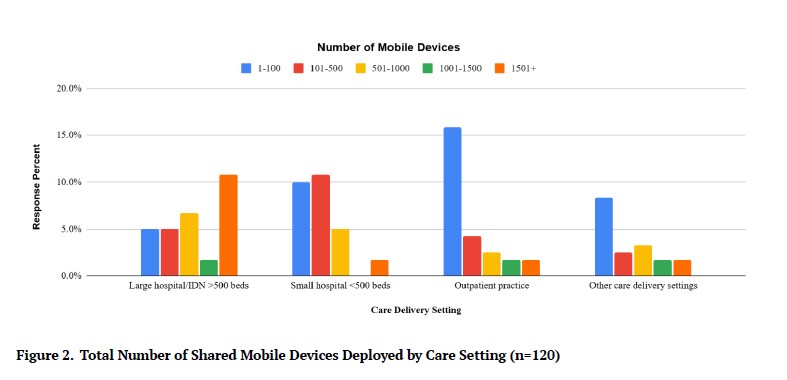
Figure 2.Total Number of Shared Mobile Devices Deployed by Care Setting (n=120)
For the question about estimated level of shared device use in their facilities/systems, almost three-fourths (150; 73.3%) of respondents estimated either an extensive (78; 38.3%) or moderate (71; 35.0%) level of shared mobile device users. Twenty percent reported having no shared-use of mobile devices, and 21.7% (44) reported limited use.
Apple iPhones and iPads were most common (114; 55.8% and 117; 57.5%, respectively), with Android devices deployed in almost 1/4 of facilities/systems (48; 23.3%). Users are required to authenticate in order to access each application among the large majority of respondent HDOs (175; 85.9%), with a majority using personal rather than shared passcodes or other credentials (105; 51.7%).
Perceived Efficiency of Mobile Devices
Respondents were asked whether they believe mobile devices are more efficient than traditional workstations for completing clinical and other tasks. Responses were mixed, with 47.5% (97) stating they were more efficient, 20.0% (41) stating that mobile devices were less efficient, and the balance stated that workstations and mobile devices are roughly equal with respect to efficiency (66; 32.5%).
Frequency of Application Use
Figure 3 displays respondents’ estimates of the number of different applications users access on shared-use mobile devices during a shift. Almost half of HDO representatives estimated that 2-4 applications (99; 48.3%) were accessed per shift, but a substantial minority accessed 5-14 applications (69; 33.7%).
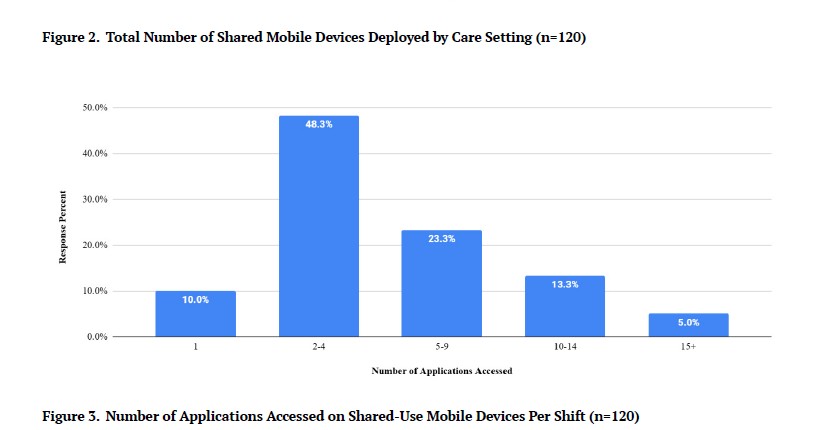
Figure 3.Number of Applications Accessed on Shared-Use Mobile Devices Per Shift (n=120)
Figure 4 shows the most frequently accessed applications on shared mobile devices. Clinical communications (141; 69.2%) and the electronic health record (EHR; 136; 66.7%) were the most frequently accessed applications.
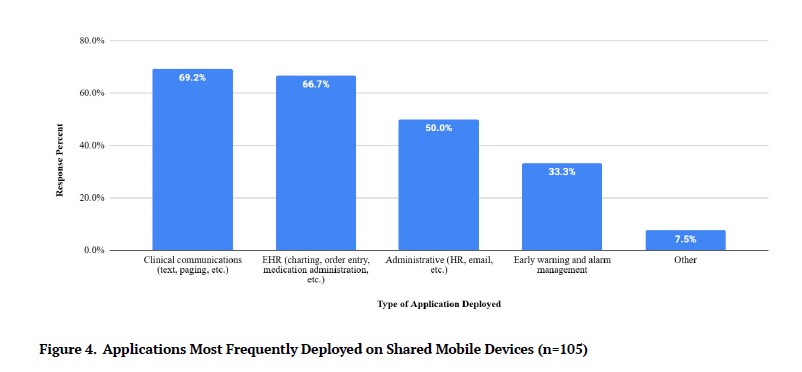
Figure 4.Applications Most Frequently Deployed on Shared Mobile Devices (n=105)
Figure 5 shows that 31.1% (63) of respondents estimated that applications were accessed more than 20 times per shift, and almost 2/3 (133; 65.1%) estimated that applications were accessed more than 10 times per shift.
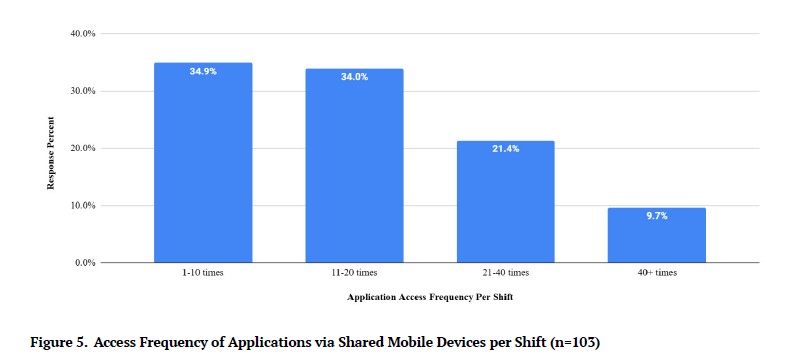
Figure 5.Access Frequency of Applications via Shared Mobile Devices per Shift (n=103)
Access Credential Processes
Eighty percent of respondents indicated that their HDO policies require users to enter credentials to unlock the device and access applications, which while adding a level of security, also introduces workflow inefficiency and a potential barrier to patient care. A minority (20; 10%) do not employ any authentication for device access, while 1/3 (67) use a shared passcode. Only 55.0% (112) utilize personal codes critical for audit trails and accountability, and 1/3 (67) use shared passcodes to access only certain applications – creating potential risk and auditing challenges as well as poor user experience.
Only 35.0% (71) of respondents felt that they never or hardly ever forget their password for mobile applications (Figure 6). More than 60% (123) of respondents reported sometimes or often forgetting their passwords to mobile applications.
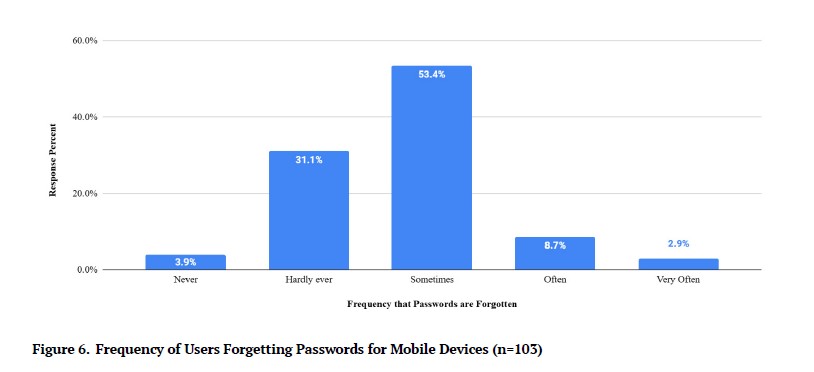
Figure 6.Frequency of Users Forgetting Passwords for Mobile Devices (n=103)
Missing or Misplaced Mobile Devices
When asked how mobile devices are exchanged or distributed among users between shifts, 44.7% (91) of respondents stated there was no defined process, while 34.0% (69) had a pre-assigned handoff between users, and 15.5% (32) used a manual process. Respondents were asked about user impact when a device is missing or misplaced. Figure 7 shows that delays in patient care and lost time were reported by almost half of respondents, and user frustration was reported by 58.3% (119).
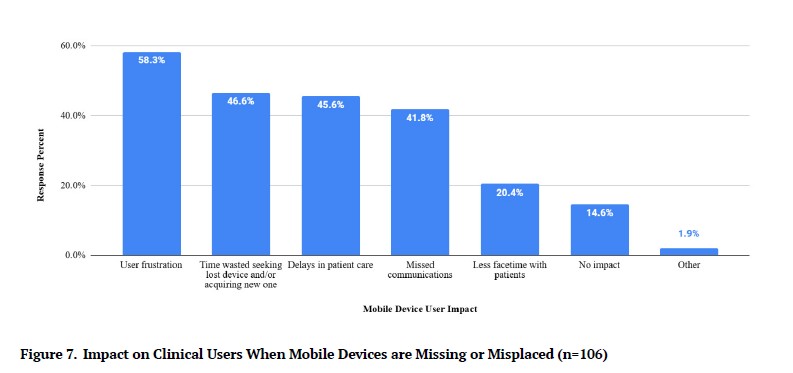
Figure 7.Impact on Clinical Users When Mobile Devices are Missing or Misplaced (n=106)
Desire for and Perceived Benefit of Greater Mobile Device Use
Interestingly, when asked whether they would like to see greater use of mobile devices by their hospital or system, only 37.2% (76) responded in the affirmative, with 41.9% (85) undecided and 20.9% (43) stating they would not. Among those stating they would like to see greater mobile device use, improved workflow efficiency, flexibility and user satisfaction were most frequently cited, along with improved communications (Figure 8).
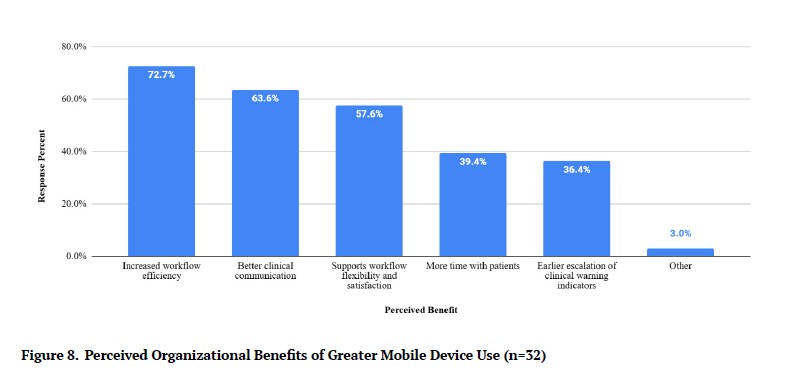
Figure 8.Perceived Organizational Benefits of Greater Mobile Device Use (n=32)
Figure 9 shows reasons respondents do not use enterprise-owned shared mobile devices, with the most commonly cited reasons being limited resources and a perceived low cost-benefit ratio.
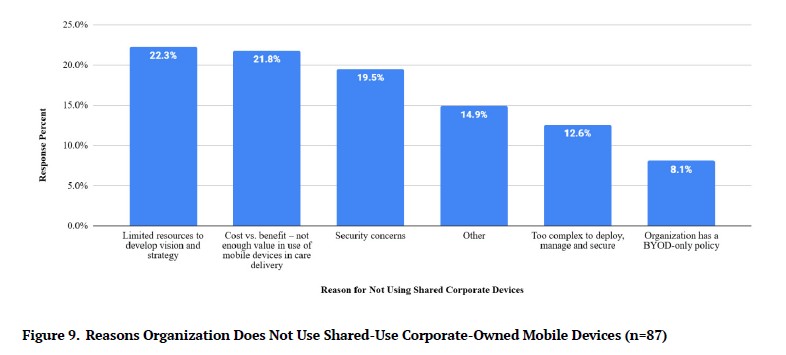
Figure 9.Reasons Organization Does Not Use Shared-Use Corporate-Owned Mobile Devices (n=87)
DISCUSSION
Respondents to this survey reported substantial mobile device use in clinical care settings driven by varied use cases and value propositions, including pursuit of increased care efficiency, desire to ensure a more seamless clinical-user experience, and need to reduce clinician loss of productivity and fatigue. Use of mobile devices in HDOs spanned across care settings, including not just large hospitals or independent delivery networks, but smaller facilities and systems as well as outpatient practices. This ubiquity by care site is somewhat surprising, as a priori one might have expected that only larger systems would have the resources to adopt mobile devices in care delivery, particularly if the devices are enterprise-owned and managed. Just over half (120; 58.7%) of respondents indicated that they deployed corporate-owned shared devices.
Mobile device integration improves communication between larger hospitals/IDNs and smaller inpatient or outpatient facilities, which frequently share patient health records, test results, and referrals; in this way, integration can improve information sharing and care coordination.13,14 Smaller facilities may be compelled to integrate mobile devices to improve communication with larger facilities and large scale healthcare networks, perhaps explaining a larger-than-expected adoption of mobile devices by smaller facilities and outpatient practices observed. This may also explain differing degrees of utilization of mobile devices based on clinical practice. Previous research has suggested that mobile devices may offer greater benefits to certain outpatient practices that rely heavily on the IoMT, such as radiology clinics.14 Thus, mobile devices can be leveraged differently yet collectively by healthcare facilities of all sizes to improve care delivery, accessibility, and communication, ultimately possibly improving integration and organization of large healthcare networks at scale.15,16
The most frequent reasons cited by respondents for why HDOs are not engaging mobility are a lack of resources to develop a mobile device vision and strategy; inability to plan effective resource use and total cost versus perceived benefit or value; inability to extract enough benefit from mobile devices to warrant the required investment; and security concerns around shared devices creating new potential vulnerabilities and threat opportunities. Fortunately, technology solutions exist which can ease HDO resource planning, shared device management, and workflows, and integrating or expanding already-implemented authentication processes to minimize security vulnerabilities. With an effective mobile access management platform in place, HDOs can derive the diverse value of shared mobile devices without sacrificing data security, user and IT management convenience, or workflow efficiency.
Technology solutions exist that enable effective and efficient management of an HDO mobile device fleet, supporting a more secure and consistent workflow. Yale New Haven Health System (YNHHS) implemented an enterprise owned shared device (EOSD) management solution by deploying Imprivata Mobile Access Management, as reported by the authors in a previous case study.8 The solution automated mobile phone provisioning, and conveyed comprehensive access control that streamlined mobile device access and authentication.8 Cloud-based management tools helped the IT team track, support and maintain mobile devices, and were integrated with the existing single sign-on solution, allowing rapid authentication processes and workflows that were already familiar to clinicians in accessing workstations, the EHR, and related applications.8 The IT team implemented authentication policies from a centralized platform that was applied across multiple systems and workflows, improving compliance while reducing ownership cost. Fewer IT resources were needed to manage mobile workflows as well as missing or lost mobile devices.8
In the previous case study,8 clinicians were able to access shared mobile devices using a proximity identity badge that eliminated the need for manual entry of credentials. The technology platform can be updated from any location. Imprivata Enterprise Access Management was also implemented for physicians accessing PHI from a personally owned mobile device to improve security using two factor authentication for remote network access, cloud applications, and Windows servers and desktops.8 Imprivata Enterprise Access Management for DEA-compliant electronic prescription of controlled substances provided extensive two-factor authentication modalities, including hands free authentication (HFA), push token notification, and convenient fingerprint biometrics.8
YNHHS benefits from their EOSD management solution by conveying comprehensive device management capabilities. Clinician user satisfaction improved, as did mobile workflows and the effectiveness of the system’s efforts to systematically manage the enterprise mobile device fleet.8 This leading academic medical center reported improved IT resource management and decreased mobile device loss. The administrative burden on the IT department was reduced, and the technology’s impact and value demonstration were apparent quickly following implementation.8
While the demand for clinical mobility seems to be increasing among HDOs in the US, the opportunities and benefits conveyed by mobile workflows still represent a challenge for both users and managers of mobile device services and functionality. Clinicians and health IT system leaders seek what mobility adds to the delivery of care and clinician experience, but managing an enterprise mobile device fleet brings complex challenges.
Mobility management tools are needed and can help with achieving rapid and easy device authentication and information access. EOSD management solutions can help HDOs improve access security and interoperability, user experience and workflow flexibility, while reducing IT administrative burden and streamlining mobile device and information access management. Mobility is becoming an integral component within the healthcare information ecosystem by enabling access to the EHR and associated informatics tools by clinicians at the bedside. This conveys more time for providers to deliver patient-centered care.
Frictionless mobility may also diminish clinician professional burnout – particularly the component which is health IT related – as workflows are expedited and made more efficient. Increased productivity and decreased stress for clinicians may improve patient experience and satisfaction indirectly as well. Clinical mobility could emerge as a standard in the practice of the highest quality healthcare across the globe. Technology solutions have been designed to help HDOs achieve these objectives, and to surmount challenges which US-based HDOs communicated in this study, including reducing expenditures for IT management of an enterprise mobile device fleet, for lost devices that require replacement, and minimizing waste in the associated downtime and work idle.
CONCLUSIONS
Mobile workflows are becoming integral to the healthcare information ecological system, enabling bedside access to the EHR and clinical applications. HDOs seek the benefits mobility can add to care delivery and clinician experience, but perceive managing an enterprise mobile device fleet as complex and challenging. Mobile access management tools are needed to streamline rapid, secure device authentication and information access with improved interoperability, user experience, and workflow flexibility while reducing the IT administrative burden of mobile device fleet management.
Disclosures
GAG and GLG are external advisors to Imprivata (Waltham, MA); RP and SPK are employees of Imprivata. Imprivata is the manufacturer of products discussed in this study.
Funding
The authors received no funding for this research.
Bibliography
-
1.
Lee M, Bin Mahmood ABS, Lee ES, Smith HE, Tudor Car L. Smartphone and mobile app use among physicians in clinical practice: Scoping review.
JMIR Mhealth Uhealth. 2023;11:e44765. doi:
10.2196/44765. PMID:37000498
-
2.
Steinhubl SR, Muse ED, Topol EJ. The emerging field of mobile health.
Sci Transl Med. 2015;7(283):283rv3. doi:
10.1126/scitranslmed.aaa3487. PMID:25877894
-
-
4.
Martin G, Khajuria A, Arora S, King D, Ashrafian H, Darzi A. The impact of mobile technology on teamwork and communication in hospitals: a systematic review.
J Am Med Inform Assoc. 2019;26(4):339-355. doi:
10.1093/jamia/ocy175. PMID:30689893
-
5.
White A, Thomas DS, Ezeanochie N, Bull S. Health worker mhealth utilization: A systematic review.
Comput Inform Nurs. 2016;34(5):206-213. doi:
10.1097/CIN.0000000000000231. PMID:26955009
-
-
7.
Bhavnani SP, Narula J, Sengupta PP. Mobile technology and the digitization of healthcare.
Eur Heart J. 2016;37(18):1428-1438. doi:
10.1093/eurheartj/ehv770. PMID:26873093
-
8.
Gellert GA, Stanton G, Paulemon M, Roberts M, Hardcastle R, Kelly SP. Challenges and opportunities in achieving secure hospital mobility management: An illustrative use case.
Journal of Hospital Administration. 2024;13:1-9. doi:
10.5430/jha.v13n2p1
-
-
10.
Hitti E, Hadid D, Melki J, Kaddoura R, Alameddine M. Mobile device use among emergency department healthcare professionals: prevalence, utilization and attitudes.
Sci Rep. 2021;11(1):1917. doi:
10.1038/s41598-021-81278-5. PMID:33479264
-
11.
Hewitt B, Dolezel D, McLeod A Jr. Mobile device security: Perspectives of future healthcare workers. Perspect Health Inf Manag. 2017;14(Winter):1c. PMID:28566992
-
12.
Gellert GA, Gellert GL, Pickering R, Kelly SP. The love-hate state of mobile device management in healthcare: An international survey.
Informatics in Medicine Unlocked. 2024;52:1-9. doi:
10.1016/j.imu.2024.101603
-
13.
Srivastava S, Pant M, Abraham A, Agrawal N. The technological growth in ehealth services.
Comput Math Methods Med. 2015;2015:894171. doi:
10.1155/2015/894171. PMID:26146515
-
14.
Gupta S, Johnson EM, Peacock JG, et al. Radiology, mobile devices, and internet of things (IoT).
J Digit Imaging. 2020;33(3):735-746. doi:
10.1007/s10278-019-00311-2. PMID:31898039
-
15.
Kraushaar J, Bohnet-Joschko S. Prevalence and patterns of mobile device usage among physicians in clinical practice: A systematic review.
Health Informatics J. 2023;29(2):14604582231169296. doi:
10.1177/14604582231169296. PMID:37063054
-
16.
Kashgary A, Alsolaimani R, Mosli M, Faraj S. The role of mobile devices in doctor-patient communication: A systematic review and meta-analysis.
J Telemed Telecare. 2017;23(8):693-700. doi:
10.1177/1357633X16661604. PMID:27632990