Download PDF
Abstract
Background
Accurate clinical documentation is essential for patient care, interdisciplinary communication, quality metrics reporting, and hospital reimbursement. Many hospitals face significant revenue losses due to inadequate or incomplete documentation.
Methods
A retrospective chart review was conducted at a 250-bed community hospital in Queens, NY, analyzing surgical coding queries from January 2021 to December 2023. Before 2021, clinical documentation improvement (CDI) queries were randomly assigned to residents or attendings. In 2021, a quality improvement initiative centralized queries to the administrative chief resident, who facilitated resolutions. Data, including query volume and response times, were extracted from 3M CDI software.
Results
A total of 701 charts were reviewed for the study period. Prior to the intervention, CDI queries averaged 18 per month with a 67% response rate within 24 hours. Following centralization in 2021, query volume decreased to 9 per month by 2023, and the 24-hour response rate improved to 97%. The implementation of standardized templates and real-time coding reviews contributed to these improvements.
Conclusions
Centralizing CDI queries and integrating structured interventions into surgical training programs significantly improved documentation accuracy and response times. Enhanced collaboration between residents and CDI specialists positively impacted workflow efficiency, patient care, and hospital financial outcomes.
Introduction
The Affordable Care Act of 2010 established programs for quality care and outcomes reporting.1 Clinical documentation reflects inpatient acuity of illness, risk of mortality, and quality of care provided, contributing to increases in the case mix index (CMI) and reimbursement.1 Clinical documentation improvement (CDI) has become an integral component of healthcare quality, supported by clinical documentation integrity specialists (CDIS).2 CDIS are often regarded as the “unsung heroes” of the healthcare industry, ensuring proper documentation for accurate hospital reimbursement.2
In teaching hospitals, residents are responsible for a significant portion of the documentation. As a result, collaboration between CDIS and resident teams is paramount. However, this presents challenges due to residents’ limited documentation experience and CDIS’ restricted clinical knowledge, leading to frequent queries and workflow interruptions.
Our surgical residency program in a 250-bed community hospital in Queens, NY (Flushing Hospital Medical Center) covers general surgery and a variety of sub-specialties. The team includes 15 residents, three physician assistants, and six faculty members, led by one administrative chief resident per quarter, supervised by faculty. Our hospital’s CDI department, established 17 years ago with five staff members, initially focused on reviewing physician documentation to capture conditions impacting illness severity. Four new members were added later as responsibilities expanded to prebill validation, appeals for diagnosis-related group (DRG) denials, and ambulatory surgery documentation.
Under our hospital’s CDI procedure, daily chart reviews are conducted to ensure documentation is clear and comprehensive and to enable accurate coding. Queries are generated in response to inconsistent, ambiguous, or incomplete chart entries, with missing laterality, chronicity, or anatomic details relevant to diagnoses or procedures. Appropriate documentation is also addressed through resident lectures provided by the CDI department three times per year (which remained the same from 2021 to 2023) to emphasize the importance of accurate documentation, health information maintenance, and their correlation with severity of illness (SOI), CMI, patient safety, and cost-effectiveness.
In 2018, the adoption of the 3M (St. Paul, Minnesota) CDI platform optimized these processes, automating case reviews and query generation while integrating coding guidelines. At our institution, a quality improvement project was undertaken to better integrate CDI into the general surgery resident workflow to improve communication and reduce CDI queries. In this article, we review the results of this quality improvement project and its impact on turnaround times and response rates.
Methods
Setting and sample
This study is a retrospective chart review of surgical coding query data from January 1, 2021 to December 31, 2023, conducted at a community hospital in Queens, NY. A total of 701 charts were reviewed. Query data was extracted by the hospital CDI team. The CDI department included nine staff members, with five dedicated to clinical documentation. Data was extracted from 3M CDI software and included the type of query (ie, procedure or progress note where data was missing, time to response, and time to resolution). This study was exempted by the hospital’s institutional review board (IRB) (exemption number 2319115-1).
Procedure
The reciprocal and interactive process of query-answer between physician and CDI staff is managed via 3M coding software and EPIC (Verona, Wisconsin) electronic medical record (EMR) software. First, clinical documentation is reviewed by CDIS, and any identified discrepancies are translated into queries and sent to the surgeon associated with the clinical documentation. A notification in the EMR signals to the provider the need to review the query and respond via the 3M platform. The identified discrepancies in missing data are linked to 3M templates specific to documentation, including, but not limited to, discrepancies related to sepsis, bedside debridement, or procedure notes. The platform generates monthly reports with aggregated data relating to number, type, and status of queries, which can be reviewed by clinical and administrative teams.
Design
This study examines changes in the coding query workflow following changes in CDIS protocol. Before 2021, the CDIS protocol called for CDI queries to be sent to any resident or attending from the surgical team who wrote a note with missing information. After a review of monthly 3M platform reports, it was observed that in the surgery department, many queries remained either unanswered or answered with a significant delay. As a result, department leadership decided to centralize queries. Beginning in 2021, all queries were sent directly to the administrative chief resident, who either personally resolved the CDIS discrepancy (eg, incomplete data) or facilitated the addition of missing details and necessary modifications.
The primary objective of this study was to assess the number of queries per month before and after centralization of queries. The secondary objective was the response time rate before and after centralization. Descriptive statistics are provided for rates of queries, query response times, and resident understanding. Rate of queries were analyzed by month and presented by year in the Figures.
Results
A total of 701 charts were reviewed for this study (223 in 2021, 271 in 2022, 207 in 2023). Before 2021, CDI queries were directed randomly to residents or attendings documenting in charts. In 2020, queries averaged 18 per month, with a 67% response rate within 24 hours. By 2023, following the protocol changes described in 2021, queries decreased to 9 per month, and the response rate within 24 hours improved to 97% (Figures 1 and 2). The initial drop in queries in 2022, to an average of 14 per month with 90% response rate, was a result of all methods being implemented, with additional improvements seen in 2023 without the need for additional interventions. A small-scale improvement effort was created around implementing mandatory lectures on clinical documentation, health information, and medicolegal fundamentals. Our lectures contributed to the decrease in the number of queries from CDI specialists and an improved response rate. Improvements in query response times and accuracy were also achieved through increased utilization of templates (which were already present in the EPIC system since 2018) and real-time modeling of DRGs to assess impacts on SOI, risk of mortality, and other metrics.
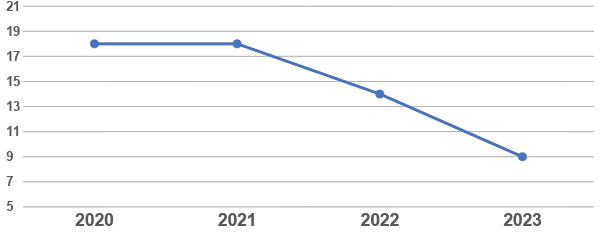
Figure 1.Comparing average number of queries per year before and after intervention.
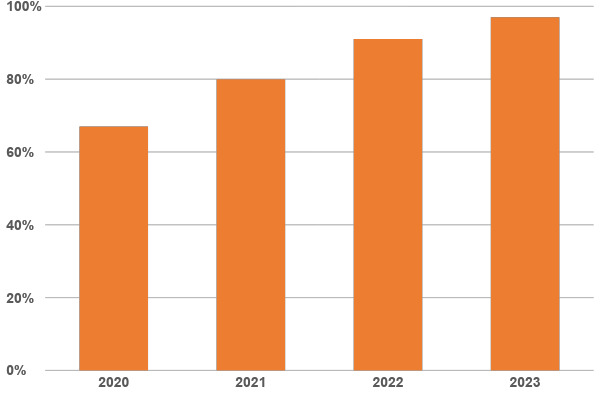
Figure 2.Comparing average response rate within 24 hours per year before and after intervention.
Discussion
The goal of surgery is the delivery of effective, efficient, and safe care. This requires data gathering, identifying where better care is needed, and assessing responses to improvement efforts.3 Clinical documentation determines inpatient acuity of illness, risk of mortality, and quality of care provided.1 Almost all inpatient hospitalizations are reimbursed based on DRGs.1 Each DRG is assigned a relative weight based on historic Centers for Medicare and Medicaid Services (CMS) claims data.1 The average relative weight for a given healthcare institution or specific patient group is the CMI.1 It is vital to determine from physician notes whether the condition requiring hospitalization has any minor or major complications, correlating to its severity and risk of mortality. Intensivists found that precise notes in medical records have a favorable outcome on quality metrics, the accuracy of administrative databases, hospital reimbursement, and perceived patient complexity.4 A 2022 study of child and adolescent psychiatrists by Khan et al at an outpatient services center revealed that comprehensive clinical documentation is indispensable for delivering high-quality care and preventing potential shortfalls.5
Inaccurate and inadequate clinical documentation results in significant revenue loss. Reimbursements have a significant impact on hospital survival. Thus, when healthcare providers accurately document patients’ charts, the hospital is reimbursed correctly, which is financially advantageous, producing a world-class health system.6,7 One survey reported an increase of at least $1.5 million in US healthcare revenue following CDI efforts.8
In the fast-paced surgical world, with daily emergencies and interventions that can limit documentation time, this concept of CDI must be emphasized early in training, at the resident level. A 2019 study by Castaldi et al reported that the surgery department of a trauma and tertiary care teaching hospital incurred almost $2 million in potential opportunities and $65,000 in lost revenues.6 A potential cause of inadequate clinical documentation was insufficient education in a 2017 pilot study of general surgery residents, prompting the use of memory aids, documentation-focused didactics, and a strict commitment to the application of guidelines.7–9
For most physicians, coding is a convoluted and intimidating process. Coders cannot infer or assume any condition without clear documentation. It is one of the most critical parts of the revenue cycle and provides an opportunity to catch early inconsistencies and prevent future errors.4 Though many clinicians have limited time and instead focus on their patients, documentation plays a critical role in correctly and accurately portraying a patient’s condition. Problems in clinical documentation include the need for resources assigned to execute a CDI program, additional administrative responsibilities, and physician burnout.4–10 The premise of CDI is to engage clinicians to improve clinical documentation in “real-time” so it is fit for reporting, analysis, and reimbursement. Poorly written notes can lead to errors in management and difficulty in defending medical malpractice claims.
The benefits of a CDI program far outweigh the pitfalls, as physicians’ engagement in documentation can highlight patients at high risk, resulting in earlier implementation of preventative measures, leading to improved patient care. This leads to faster discharges, fewer readmissions, and financial benefits to increase case mix and coding standard compliance.4–10
Future physicians receive limited teaching on clinical documentation during medical school. This requires on-the-job training with feedback from residents, ensuring high-quality, accurate, and concise notes.11–13 Educational sessions using a formal documentation curriculum, templates, and routine note assessment and feedback improve documentation. A 2016 study by Kittinger et al at the Division of Plastic Surgery at Baylor Scott & White Memorial Hospital in Texas demonstrated that complete comprehension of clinical documentation, especially coding and billing, is essential to practicing medicine and effective patient care.12 At our institution, our department identified the problem that needed to be fixed through the data gathered: the high number of queries. The interactions between residents and the CDIS in our institution contributed to creating a friendly collaboration in which each group, focusing on the patient, understood and respected the value of their work. Consequently, proper documentation provided dividends for patient care, workflow, and teamwork, with appropriate use of resources, skills, and energy in an organized approach. The impact of initiatives to CDI can also be evaluated through additional outcome parameters such as severity of illness (SOI), risk of mortality (ROM), revenue cycle return on investment (ROI), CMI, all-payer refined diagnosis-related groups (APR-DRG), and surgical care improvement program (SCIP) metrics. In the future, based on 3M reporting, we plan to capture conditions and missing information most frequently queried, and those with the longest response turnaround time to build templates and teaching sessions to further improve documentation.
Limitations
This was a single-center study; our focus was on decreasing queries through better documentation. We did not review increases in surgical SOI, ROM, CMI, APR-DRG, support resources used or the financial impacts of reimbursement charges or outcome measures.
Conclusions
CDIS-physician integration into the resident team can occur through a collaborative focus with simple interventions, leading to a better understanding of the impact of clinical documentation on patient safety and quality of care. Although the documentation process can seem overwhelmingly complex, we have shown that simple interventions can have significant effects, as seen in the improvement of response rate from 67% before 2021 with an average of 18 queries per month, to 97% in 2023 with an average of 9 queries per month. Focusing on a handful of common specialty-specific conditions, identifying errors, and providing instructions for appropriate documentation in real-time can promptly correct and update documentation effectively.
Funding
The authors received no funding for this research.
Disclosures
The authors have nothing to disclose.
Bibliography
-
1.
Aiello FA, Judelson DR, Durgin JM, et al. A physician-led initiative to improve clinical documentation results in improved health care documentation, case mix index, and increased contribution margin.
J Vasc Surg. 2018;68(5):1524-1532. doi:
10.1016/j.jvs.2018.02.038
-
-
3.
Ko CY, Martin G, Dixon-Woods M. Three Observations for Improving Efforts in Surgical Quality Improvement.
JAMA Surg. 2022;157(12):1073-1074. doi:
10.1001/jamasurg.2022.3122
-
4.
Sanderson AL, Burns JP. Clinical Documentation for Intensivists: The Impact of Diagnosis Documentation.
Critical Care Medicine. 2020;48(4):579-587. doi:
10.1097/ccm.0000000000004200
-
5.
Khan YS, Albobali Y, Kamal LF. Improving the quality of structured clinical documentation in a child and adolescent psychiatry outpatient service: Findings from an audit cycle.
Asian J Psychiatry. 2022;77:103268. doi:
10.1016/j.ajp.2022.103268
-
6.
Castaldi M, McNelis J. Introducing a Clinical Documentation Specialist to Improve Coding and Collectability on a Surgical Service.
J Healthc Qual. 2019;41(3):e21-e29. doi:
10.1097/JHQ.0000000000000146
-
7.
Garcia A, Revere L, Sharath S, Kougias P. Implications of Clinical Documentation (In)Accuracy: A Pilot Study Among General Surgery Residents.
Hosp Top. 2017;95(2):27-31. doi:
10.1080/00185868.2017.1300471
-
-
9.
Tanveer S, Khilji M, Gul N, et al. Enhancing Documentation Precision in Ophthalmic Surgery: A Quality Improvement Project.
Cureus. 2023;15(12):e51274. doi:
10.7759/cureus.51274
-
10.
Shepheard J. What do we really want from clinical documentation improvement programs?
Health Inf Manag. 2018;47(1):3-5. doi:
10.1177/1833358317712312
-
11.
Rowlands S, Coverdale S, Callen J. Documentation of clinical care in hospital patients’ medical records: A qualitative study of medical students’ perspectives on clinical documentation education.
Health Inf Manag. 2016;45(3):99-106. doi:
10.1177/1833358316639448
-
12.
Kittinger BJ, Matejicka A 2nd, Mahabir RC. Surgical Precision in Clinical Documentation Connects Patient Safety, Quality of Care, and Reimbursement. Perspect Health Inf Manag. 2016;13(Winter):1f.
-
13.
Cromwell PM, Flood M, O Connell E, et al. POST-OP: A Strategy to Improve Clinical Documentation in the Early Postoperative Period.
J Surg Educ. 2018;75(4):957-963. doi:
10.1016/j.jsurg.2018.01.005