Download PDF
Abstract
Background
Clinical Documentation Integrity (CDI) programs aid in documentation of precise diagnoses. In this study, the authors assessed the rate at which certain diagnoses were present in the Pediatric Health Information System (PHIS) database and evaluated changes in the hospital-specific case mix index (CMI) pre- and post-CDI program inception at six children’s hospitals.
Methods
Between 2011 and 2017, CDI programs were implemented at six children’s hospitals. The authors queried the PHIS database to compare the following diagnoses in 2010 and 2021: acute respiratory failure, chronic respiratory failure, ventilator dependence, dysphagia, malnutrition, and presence of a gastrostomy and/or jejunostomy (G/J) tube in patients with aspiration.
Results
From 2010 to 2021, CMI increased at all hospitals. For all hospitals’ inpatient encounters, the percentage of patients with acute respiratory failure and malnutrition increased (both p <0.001). Documentation of chronic respiratory failure increased (p < 0.001) and ventilator dependence decreased (p < 0.001) at all institutions. There were variations at the hospital level for capture of dysphagia, G/J and both diagnoses together.
Conclusions
CMI increased and the rate of specific diagnoses in the PHIS database increased from 2010 to 2021, which corresponded to implementation of all institutions’ CDI programs. Documentation of specific, clinically-relevant diagnoses in the medical record ensures optimal healthcare provider communication, proper severity of illness representation, appropriate hospital reimbursement, accurate quality metric reporting and database accuracy.
Introduction
Inaccurate or missing diagnoses in the medical record can lead to gaps in communication amongst healthcare providers, potentially negatively affecting patient care.1–3 Physicians may use symptom descriptors or imprecise diagnoses rather than specific diagnoses,4 which can result in inexact coding. Consequently, patient complexity may be underrepresented, hospital reimbursement may be suboptimal, quality metric reporting may be erroneous, and research databases may be inaccurate.
The All Patient Refined Diagnosis Related Group (APR-DRG) system is one methodology used in the pediatric population to determine patient complexity and hospital reimbursement. Patients are assigned to specific DRGs, then automatically assigned one of four severity of illness (SOI) subclasses and one of four risk of mortality (ROM) subclasses.5 Certain diagnoses are more heavily weighted than others and can increase the SOI and ROM levels. A numeric value, the relative weight (RW), is assigned to each DRG; higher levels of SOI increase the RW, since sicker, more complex patients are expected to utilize more resources. As such, facility reimbursement is linked to the relative weights of a hospital’s patient population, the average of which is represented by the case mix index (CMI). Since the APR-DRG system relies upon documentation of specific diagnoses and procedures, suboptimal documentation may lead to an incorrect reflection of patient complexity.
Clinical Documentation Integrity (CDI) programs have been implemented at many institutions to aid in physician documentation of precise diagnoses. CDI specialists are professionals who clarify alternate, imprecise, inaccurate, or missing diagnoses from the medical record in the form of queries to physicians and advance practice clinicians. CDI programs also provide educational opportunities and tools via didactic lectures, tip cards, and note templates.6–8 Institutions have demonstrated increases in patient complexity as well as facility reimbursement with the assistance of their CDI program.9–12
Patients with ventilator dependence have chronic respiratory failure but clinicians may only document one or the other in the medical record. Ideally, clinicians should document both diagnoses, as this more accurately demonstrates the complexity of the patient population compared with only documenting one of these diagnoses alone. Acute respiratory failure occurs when oxygenation and/or ventilation is insufficient to meet the metabolic demands of the body and may be classified as hypoxemic and/or hypercapneic. Anecdotally, acute respiratory failure is under-documented because clinicians may use less specific terminology, non-intensivists may assume that respiratory failure must be treated in an intensive care unit, or physicians may feel diagnosing acute respiratory failure is beyond their scope of practice.13
Failure to thrive (FTT) and malnutrition are commonly used interchangeably, even though these diagnoses are not identical. FTT is lack of expected growth in children less than three years of age. Although FTT is due to undernutrition in most cases, the etiology may be medical conditions not related to nutritional intake.14 Malnutrition is an imbalance between nutrient requirements and intake, and it may result in underweight, stunting, and/or wasting.15 In addition to affecting growth, malnutrition can also affect other outcomes such as muscle strength, immune function, motor and speech development, and cognition.16
Patients with dysphagia may aspirate food, liquids, and/or secretions, requiring a gastrostomy and/or jejunostomy tube (G/J) to safely feed. In these situations, it is important for physicians to document both dysphagia and the presence of a G/J to fully capture the complex nature of the patient’s medical condition.
The objective of this study was to assess the rate at which certain diagnoses were present in the Pediatric Health Information System (PHIS) database before and after establishing CDI programs at six freestanding children’s hospitals. In addition, we sought to evaluate changes in the hospital-specific CMI at our respective institutions. We hypothesized that after CDI program inception, there would be an increase in individual hospital CMI and better capture of certain specific diagnoses that impact patient complexity representation.
Methods
Setting
Between 2011 and 2017, CDI programs were implemented at Boston Children’s Hospital (BCH), Children’s Hospital Los Angeles (CHLA), Children’s Hospital of Philadelphia (CHOP), Children’s Nebraska (CNEB), Johns Hopkins All Children’s Hospital (JHACH), and Phoenix Children’s Hospital (PCH). Institutional size ranged from 225 (CNEB) to 535 beds (CHOP).
Study Design
We conducted a multicenter, retrospective cohort study of pediatric inpatients using administrative data from the PHIS for years 2010 and 2021. PHIS is a comparative database that contains clinical and resource utilization data from 50 pediatric hospitals and is maintained by the Children’s Hospital Association (Lenexa, KS).17 Diagnoses present in the database are based on International Classification of Diseases (ICD) codes derived from billing charges (ICD-9 for 2010 and ICD-10 for 2021), which are based on documentation. Therefore, for the purposes of this study, we used the presence of a diagnosis in the PHIS database as a proxy for documentation in the medical record. A certified medical coder verified appropriate application of ICD codes (Supplemental Table). Institutional review board approval was not required, as this project utilized de-identified administrative data and therefore did not constitute human subject research.
We queried the PHIS database to compare the following diagnoses in 2010 and 2021: chronic respiratory failure, ventilator dependence, dysphagia, presence of a G/J in patients with aspiration, malnutrition, and acute respiratory failure. Regarding dysphagia and G/J, we evaluated patients with a diagnosis of aspiration because if a G/J is indicated, then dysphagia is likely present. We also obtained hospital-specific CMI data as well as the number of hospital inpatient visits from the PHIS database for 2010 and 2021.
Statistical Analysis
Categorical diagnosis-based impact groups were summarized using frequencies, percentages, and 95% confidence intervals; they were compared between 2010 and 2021, on the hospital level, by Pearson chi-squared (χ2) tests. All statistical analyses were performed using Stata software version 18.0 (StataCorp LLC, College Station, TX). A two-tailed 5% alpha level was implemented and p-values less than 0.05 were considered statistically significant.
Results
Hospital Inpatient Encounters
Comparing 2010 to 2021, the number of hospital inpatient visits increased for four of the six hospitals: BCH (20,971 to 22,157), CHLA (11,404 to 17,036), CNEB (7,412 to 7,842) and PCH (14,380 to 18,213). During the same years, the number of inpatient visits decreased for CHOP (28,975 to 27,934) and JHACH (12,200 to 8,176). The length of stay and major diagnostic categories did not change considerably between 2010 and 2021 for all hospitals included in the analysis (Table 1). Of note, PCH was not included, as it was no longer participating in the PHIS database at the time this specific analysis was done.

Table 1.Length of stay, relative weight and major diagnostic category 2010 vs. 2021
Case Mix Index
Based on APR-DRG version 32, the LOS-based CMI increased for all hospitals when comparing 2010 to 2021: BCH from 1.34 to 1.57, CHLA from 1.79 to 1.84, CNEB from 1.39 to 1.57, CHOP from 1.17 to 1.64, JHACH from 1.46 to 2.18, and PCH from 1.34 to 1.58.
Acute Respiratory Failure
There was an increase in the percentage of patients with acute respiratory failure for each individual hospital in 2021 compared with 2010 (Figure 1). The diagnosis of acute respiratory failure increased from 1.25% to 5.35% (p <0.001) for inpatient stays in all hospitals combined. The impact of an acute respiratory failure query is demonstrated in Table 2.
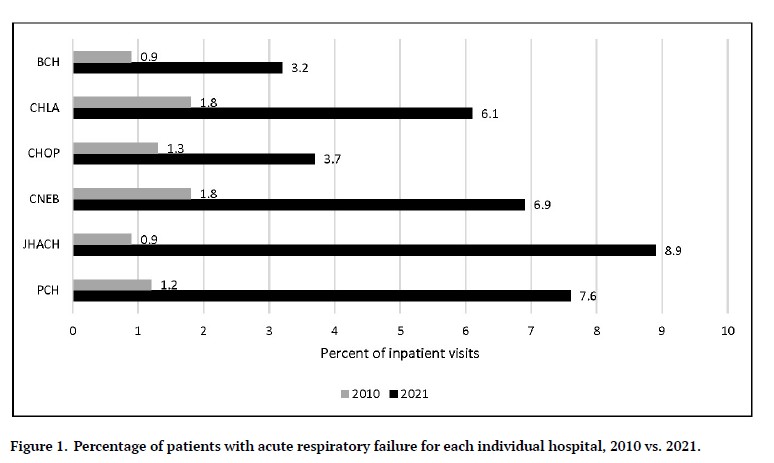
Figure 1.Percentage of patients with acute respiratory failure for each individual hospital, 2010 vs. 2021.
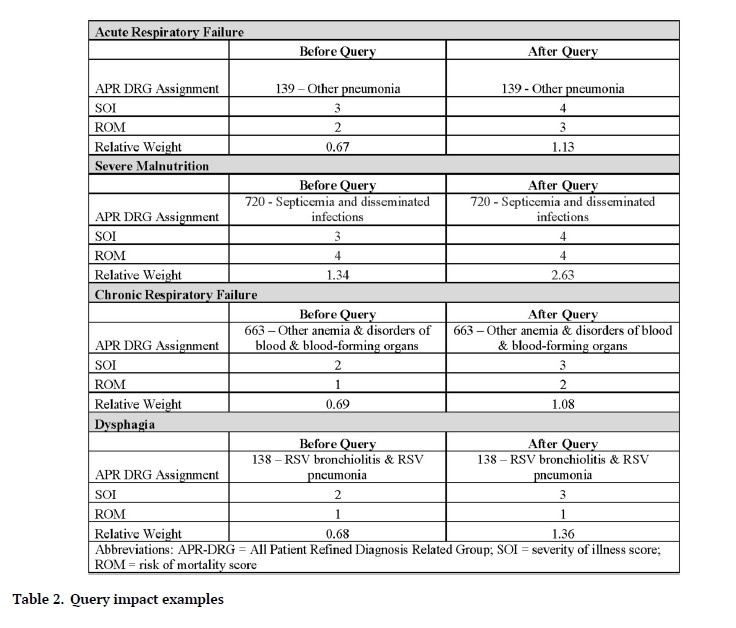
Table 2.Query impact examples
Malnutrition
From 2010 to 2021, there was an increase in the percentage of patients with malnutrition for each individual hospital (Figure 2). For inpatient hospitalizations for all hospitals combined, the diagnosis of malnutrition increased from 0.66% to 7.58% (p <0.001). The effect of a severe malnutrition query is shown in Table 2.
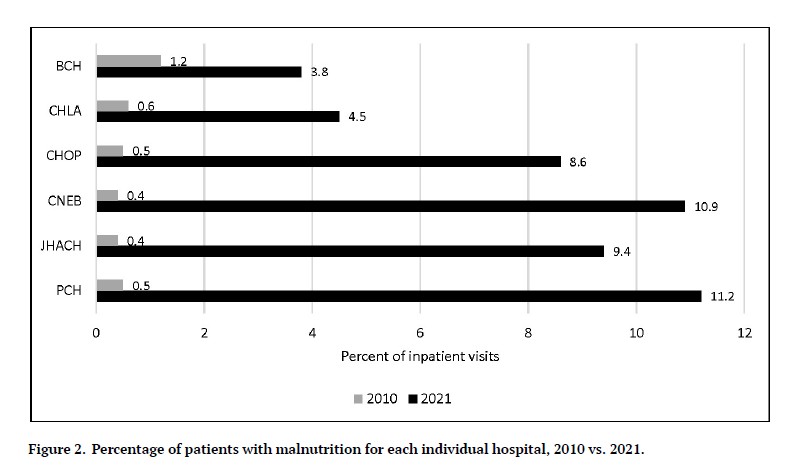
Figure 2.Percentage of patients with malnutrition for each individual hospital, 2010 vs. 2021.
Chronic Respiratory Failure and Ventilator Dependence
The frequency with which chronic respiratory failure, ventilator dependence, and both diagnoses together were present in the PHIS database are reported in Figure 3. Of note, PCH was not included in this analysis because the hospital was no longer participating in the PHIS database at the time this specific analysis was done. Individually, chronic respiratory failure increased (p < 0.001) and ventilator dependence decreased (p < 0.001) at all institutions. There was an increase in capture of both chronic respiratory failure and ventilator dependence at BCH (p < 0.001), CNEB (p < 0.001) and JHAC (p = 0.001). There was a decrease in the documentation of both diagnoses together at CHLA (p < 0.001) and CHOP (p = 0.009). The result of a chronic respiratory failure query is displayed in Table 2.
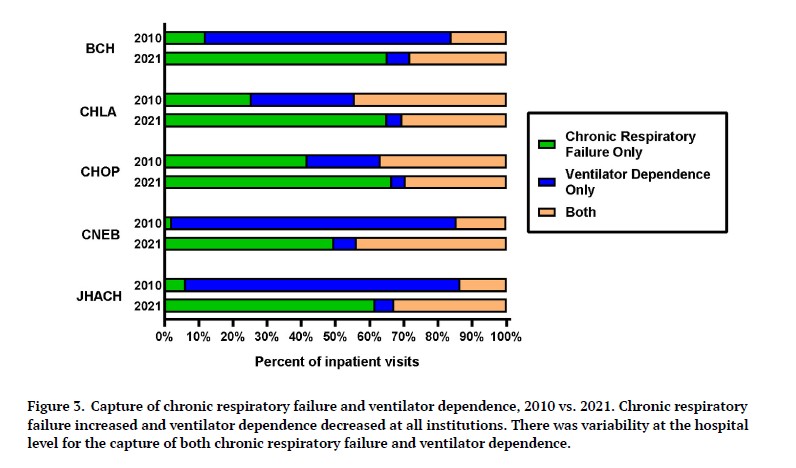
Figure 3.Capture of chronic respiratory failure and ventilator dependence, 2010 vs. 2021. Chronic respiratory failure increased and ventilator dependence decreased at all institutions. There was variability at the hospital level for the capture of both chronic respiratory failure and ventilator dependence.
Dysphagia and Gastrostomy/Jejunostomy Tube
The presence of dysphagia, G/J, and both diagnoses together in patients with aspiration within the PHIS database is presented in Figure 4. There was an increase in capture of dysphagia only at CHOP (p = 0.007) and a decrease at PCH (p = 0.01). G/J alone decreased at BCH, CHLA, and CHOP, all with p < 0.001. Documentation of both dysphagia and G/J together increased at BCH, CHLA, and CHOP (all with p <0.001). The effect of a dysphagia query is displayed in Table 2.
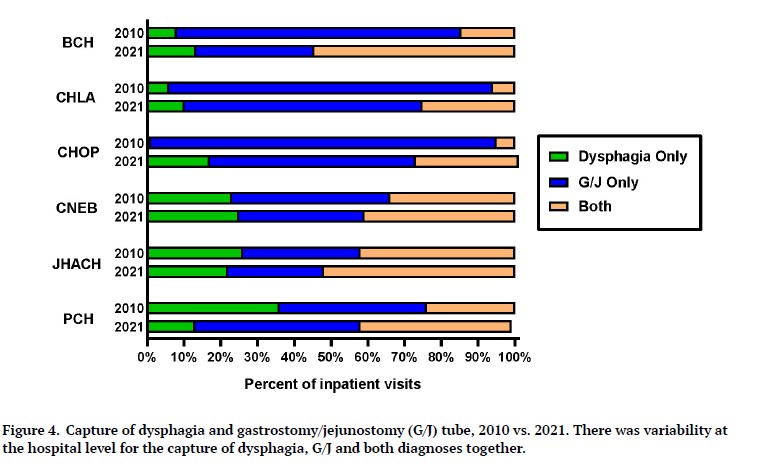
Figure 4.Capture of dysphagia and gastrostomy/jejunostomy (G/J) tube, 2010 vs. 2021. There was variability at the hospital level for the capture of dysphagia, G/J and both diagnoses together.
Discussion
We sought to assess the rate of certain diagnoses being present in the PHIS database pre- and post-CDI program inception at six freestanding children’s hospitals. Notably, we found an overall increase in the presence of diagnoses that can impact patient complexity representation and hospital-specific CMI after implementation of an intervention designed to improve the documentation of clinically relevant, specific diagnoses, a finding consistent with previous studies.6,10,18 In particular, our study expands upon the findings of a previous single center pediatric study that evaluated diagnosis documentation related to introduction of a CDI program.11 To our knowledge, this is the first multi-institutional pediatric study assessing the impact of CDI programs on diagnosis documentation.
Case Mix Index
CMI and the rate of specific diagnoses in the PHIS database increased from 2010 to 2021. Although various factors can affect CMI, such as change in patient population or types of procedures performed, we found that length of stay as well as major diagnostic categories did not change substantially. This supports our hypothesis that implementation of CDI programs at our institutions could have contributed to the increases in CMI, rather than changes in patient-specific factors.
Acute respiratory failure
We found that capture of acute respiratory failure increased significantly during our study period. Although a causal relationship cannot be established based on our study design, our findings suggest that our CDI programs made an impact in this area as this diagnosis was prioritized for queries and education.
Malnutrition
We found that documentation of malnutrition significantly increased after inception of CDI programs at all six hospitals. The increase in documentation of malnutrition was likely due to several factors: an increase in malnutrition queries, collaboration with dieticians to promote consistent notation of malnutrition in consult notes, intensive educational efforts, clinical pathway implementation and, at one hospital, introduction of an automated query process for malnutrition.
Chronic respiratory failure and ventilator dependence
We found that chronic respiratory failure and ventilator dependence separately increased and decreased, respectively, at all institutions. However, we found that documentation of both chronic respiratory failure and ventilator dependence together decreased at two of our hospitals. Chronic respiratory failure rather than ventilator dependence has been a priority for the CDI programs, which could explain these findings.
Dysphagia and presence of a gastrostomy/jejunostomy tube
Our study demonstrated an increase in documentation of both dysphagia and G/J at only half of the hospitals. Variability in results could be due to CDI programs targeting different diagnoses for education. In addition, CNEB and JHACH had small sample sizes, which could have contributed to the lack of an effect.
Limitations
Our study does have some noteworthy limitations. All six institutions are freestanding academic children’s hospitals, which could limit generalizability. Documentation habits of pediatric clinicians at community hospitals in this context are not known. Nonetheless, there is diversity amongst our institutions in size, specialization, and geography. Querying an administrative database necessitated the use of billing data as a proxy for documentation of diagnoses. There is the possibility that diagnoses were documented but not present in the PHIS database for other reasons, such as missing administrative records or coding errors. However, studies have shown that the quality of coded data is more likely to be influenced by physician documentation rather than coding errors or individual coder characteristics.19–22 It is possible that we underestimated the effect of CDI programs by omitting certain diagnoses or patient populations. Conversely, we might have overestimated the effect of our CDI programs, as there could have been other reasons for increased capture of these diagnoses and hospital CMI, such as shifts in patient populations, introduction of new procedures or other documentation interventions. However, length of stay and major diagnostic category information did not change substantially during our study period, implying large shifts in patient population did not occur. Likewise, Willer et al23 demonstrated a substantial increase in the proportion of bronchiolitis patients diagnosed with acute respiratory failure from 2010 to 2019 despite stable and improved outcomes, suggesting that higher patient acuity was not responsible for these findings. Furthermore, our CDI programs have demonstrated direct increases in patient complexity measures after clarification of imprecise or missing diagnoses from the medical record of individual patients, supporting our hypothesis that our CDI programs contributed to increased hospital CMI.
Conclusions
Our diagnoses of interest increased in the PHIS database from 2010 to 2021. Our findings support the concept that pediatric CDI programs can improve documentation of specific, clinically relevant diagnoses in the medical record, which helps to ensure proper severity of illness representation, expected length-of-stay metrics, hospital reimbursement, quality metric reporting, healthcare provider communication, database accuracy, and optimal staffing models for attending physicians. Multi-institutional intervention studies would be helpful for measuring the direct effect of pediatric CDI programs on the accurate and complete documentation of diagnoses in the medical record.
Acknowledgments
The authors would like to thank Tiffany Lott, MHA, RHIA for her thorough review and verification of the appropriate application of ICD codes for this study.
Disclosure Statement
AB is the Chief Executive Officer of Pediatric Resource Group and ALS, WA, and DPC are Consulting Associates with Pediatric Resource Group. The remaining authors have nothing to disclose.
Funding Statement
The authors received no funding for this research.
Bibliography
-
1.
Carmody JB, Swanson JR, Rhone ET, Charlton JR. Recognition and reporting of AKI in very low birth weight infants.
Clin J Am Soc Nephrol. 2014;9(12):2036-2043. doi:
10.2215/CJN.05190514
-
2.
Tsopra R, Wyatt JC, Beirne P, et al. Level of accuracy of diagnoses recorded in discharge summaries: A cohort study in three respiratory wards.
J Eval Clin Pract. 2019;25(1):36-43. doi:
10.1111/jep.13020
-
3.
Brady CC, Thaker VV, Lingren T, et al. Suboptimal Clinical Documentation in Young Children with Severe Obesity at Tertiary Care Centers.
Int J Pediatr. 2016;2016:4068582. doi:
10.1155/2016/4068582
-
4.
Vivtcharenko VY, Ramesh S, Dukes KC, et al. Diagnosis Documentation of Critically Ill Children on Admission to a Pediatric Intensive Care Unit.
Pediatr Crit Care Med. Published online 2021. doi:
10.1097/PCC.0000000000002812. PMID:34534163
-
-
6.
Kulkarni D, Heath J, Kosack A, Jackson NJ, Crummey A. An Educational Intervention to Improve Inpatient Documentation of High-risk Diagnoses by Pediatric Residents.
Hosp Pediatr. 2018;8(7):430-435. doi:
10.1542/hpeds.2017-0163
-
7.
Newnham AL, Hine C, Rogers C, Agwu JC. Improving the quality of documentation of paediatric post-take ward rounds: the impact of an acrostic.
Postgrad Med J. 2015;91(1071):22-25. doi:
10.1136/postgradmedj-2013-132534
-
8.
Spellberg B, Harrington D, Black S, Sue D, Stringer W, Witt M. Capturing the diagnosis: an internal medicine education program to improve documentation.
Am J Med. 2013;126(8):739-743e1. doi:
10.1016/j.amjmed.2012.11.035
-
9.
Morrison RJ, Malloy KM, Bakshi RR. Improved Comorbidity Capture Using a Standardized 1-Step Quality Improvement Documentation Tool.
Otolaryngol Head Neck Surg. 2018;159(1):143-148. doi:
10.1177/0194599818764669
-
10.
Reyes C, Greenbaum A, Porto C, Russell JC. Implementation of a Clinical Documentation Improvement Curriculum Improves Quality Metrics and Hospital Charges in an Academic Surgery Department.
J Am Coll Surg. 2017;224(3):301-309. doi:
10.1016/j.jamcollsurg.2016.11.010
-
11.
Reardon KE, Foley CM, Melvin P, Agus MSD, Sanderson AL. Impact of a Clinical Documentation Integrity Program on Severity of Illness of Expired Patients.
Hosp Pediatr. 2021;11(3):298-302. doi:
10.1542/hpeds.2020-000851
-
12.
Peralta J, Ham SW, Magee GA, et al. Impact of a care delivery redesign initiative for vascular surgery.
J Vasc Surg. 2020;71(2):599-608e1. doi:
10.1016/j.jvs.2019.03.053
-
-
14.
Gahagan S. Failure to thrive: a consequence of undernutrition.
Pediatr Rev. 2006;27(1):e1-11. doi:
10.1542/pir.27-1-e1
-
-
16.
Mehta NM, Corkins MR, Lyman B, et al. Defining pediatric malnutrition: a paradigm shift toward etiology-related definitions.
JPEN J Parenter Enteral Nutr. 2013;37(4):460-481. doi:
10.1177/0148607113479972
-
-
18.
Elkbuli A, Godelman S, Miller A, et al. Improved clinical documentation leads to superior reportable outcomes: An accurate representation of patient’s clinical status.
Int J Surg. 2018;53:288-291. doi:
10.1016/j.ijsu.2018.03.081
-
19.
Burles K, Innes G, Senior K, Lang E, McRae A. Limitations of pulmonary embolism ICD-10 codes in emergency department administrative data: let the buyer beware.
BMC Med Res Methodol. 2017;17(1):89. doi:
10.1186/s12874-017-0361-1
-
20.
Hennessy DA, Quan H, Faris PD, Beck CA. Do coder characteristics influence validity of ICD-10 hospital discharge data?
BMC Health Serv Res. 2010;10:99. doi:
10.1186/1472-6963-10-99
-
21.
So L, Beck CA, Brien S, et al. Chart documentation quality and its relationship to the validity of administrative data discharge records.
Health Informatics J. 2010;16(2):101-113. doi:
10.1177/1460458210364784
-
22.
Cheng P, Gilchrist A, Robinson KM, Paul L. The risk and consequences of clinical miscoding due to inadequate medical documentation: a case study of the impact on health services funding.
Health Inf Manag. 2009;38(1):35-46. doi:
10.1177/183335830903800105
-
23.
Willer RJ, Coon ER, Harrison WN, Ralston SL. Trends in Hospital Costs and Levels of Services Provided for Children With Bronchiolitis Treated in Children’s Hospitals.
JAMA Netw Open. 2021;4(10):e2129920. doi:
10.1001/jamanetworkopen.2021.29920