Download PDF
Abstract
Background
An individual’s racioethnicity can affect their use of digital health tools and access to digital resources. In this study, the authors examine the relationship between community Social Determinants of Health (cSDoH) and racioethnicity with access and use of online medical records.
Methods
Data were used from the Health Information National Trends Survey (HINTS)—specifically, HINTS 5 Cycle 1 (2017), HINTS 5 Cycle 2 (2018), HINTS 5 Cycle 3 (2019), HINTS 5 Cycle 4 (2020). Predicted probabilities of accessing online medical records based on interactions of cSDoH and racioethnicity were estimated using adjusted weighted logistic regression. Among online medical record users, the authors explored how they accessed the Internet by racioethnicity and cSDoH.
Results
A combined analytical dataset was created with 16,092 pooled observations from all four HINTS 5 cycles, including 14,103 respondents who answered a question about whether they accessed their online medical record (with 5,766 responding yes). From a range of predicted probabilities between 0 and 1, Hispanic, Non-Hispanic (NH) Black, and NH White communities had predicted probabilities for accessing online medical records of 0.20, 0.33, and 0.38, respectively, in the most disinvested neighborhoods. We also found differences in how individuals accessed their online medical record by racioethnicity and cSDoH.
Conclusions
Results suggest that incorporating cSDoH and racioethnicity in digital health decision making may help bridge the digital divide. Further research should explore the complex interplay between cSDoH, racioethnicity, online medical record access and use to promote digital health equity.
INTRODUCTION
Patient attributes, such as racioethnic identity (or one’s race and ethnicity), can collectively contribute to health outcomes.1–3 Socioeconomic and environmental conditions in one’s community4 or community Social Determinants of Health (cSDoH) can also contribute to health inequities and reflect the environment in which one lives, plays, and works.5 Intersectionality is a theoretical framework that examines how complex factors (e.g., race, class, gender) interact with one another.6–8 Intersectionality can be used to help explain health disparities and inequities.1,9 An intersectional view on the combined effect of racioethnicity and community provides an opportunity to learn about disparities in digital health technology, which has been demonstrated to have a positive contribution to health and health equity.10
An individual’s racioethnicity can affect their use of digital health tools and access to digital resources. Studies have indicated lower patient portal use and access to digital resources (e.g., broadband Internet) among communities marginalized due to racioethnicity.11,12 Factors such as digital redlining, or deliberate limiting of access to digital resources and services, have contributed to these digital inequities.13,14 Increasing digital technology in the healthcare space may worsen health disparities if digital inclusion is not considered.15,16 For instance, applications for food, housing, or employment related programs may be only offered online,17 and ideally via an online medical record as health systems are increasingly involved in the collection and management of unmet social needs.18,19
Based on the extant literature, it is known that communities marginalized by racioethnicity have lower use of online medical records.18,20 However, the health implications for these individuals across different communities are unclear.21 There is limited research on the intersection of racioethnicity with cSDoH as it pertains to online medical records use at the national level. Examining this intersection can provide valuable insights on how we can better serve individuals who live in different types of communities. This can help reduce the digital divide or “the gap between those able to easily access digital health services and those that cannot.”22 Existing literature has indicated that the digital divide persists among communities that are marginalized by racioethnicity, despite efforts to promote Internet access in the United States.23 Thus, national-level data is necessary to address these challenges and gain a deeper understanding of the contributing factors to these disparities. We leveraged data from the Health Information National Trends Survey (HINTS), a national survey that collects a variety of health information, to investigate the intersectionality between racioethnicity and cSDoH and to obtain national estimates, which is a first of its kind to provide formative evidence on digital inclusion at the national level.
METHODS
This study used data from HINTS, sponsored by the National Cancer Institute (NCI). HINTS represents a sample of individuals over 18 years of age in the United States. Individuals report how they obtain and use health information, such as healthcare access and health outcomes. This study used data from HINTS 5 Cycle 1 (2017), HINTS 5 Cycle 2 (2018), HINTS 5 Cycle 3 (2019), HINTS 5 Cycle 4 (2020). Stratified postal address frames are used to randomly sample residential addresses. HINTS uses survey weights to increase generalizability to the population.24
Predictors
Our predictors were cSDoH and racioethnicity. Racioethnicity was assessed by the HINTS question, “What is your race? One or more categories may be selected.” Answer options were "White," “Black or African American,” “American Indian or Alaska Native,” “Asian Indian,” “Chinese,” “Filipino,” “Japanese,” “Korean,” “Vietnamese,” “Other Asian,” “Native Hawaiian,” “Guamanian or Chamorro,” “Samoan,” and “Other Pacific Islander.” We recoded racioethnicity into four categories: non-Hispanic (NH) White, NH Black, Hispanic, or NH Other. To quantify cSDoH, we used ZIP codes and Area Deprivation Index (ADI) ranking data from all 50 states using the University of Wisconsin-Madison Neighborhood Atlas.25 We chose to use 2020 data from the Neighborhood Atlas since it aligned the most with the HINTS 5 cycles. ADI is a measure that considers multiple community-level factors such as income, housing, and education. ADI rankings range from 1 to 100. The higher the ADI ranking, the more disinvested the neighborhood.25 This master dataset with the cSDoH was merged to our HINTS data based on ZIP code. ADI rankings were categorized into quintiles.
Outcome
Our primary outcome was whether the individual accessed their online medical record. This was assessed by the HINTS question, “How many times did you access your online medical record in the last 12 months?” with options of “None,” “1 to 2 times,” “3 to 5 times,” “6 to 9 times,” and “10 or more times.” Options other than “None” were recoded to "Yes," and “None” was recoded to “No.” There were 1,989 respondents (12.36% of total observations) with missing data or who were unable to answer this question.
Covariates
Clinical and sociodemographic characteristics used as covariates included gender (male or female), age (18–34, 35-49, 50–64, 65-75, 75+), education (high school graduate or less, some college/bachelor’s degree, or college graduate), metropolitan status (metropolitan area or non-metropolitan area), general health (excellent/very good/good, fair, or poor), health insurance status (insured or uninsured), and Internet access (yes or no). These variables were selected because they align with previous studies on online medical records.26,27
Data and Analytical Plan
A logistic regression model was used with population weights to estimate the likelihood of accessing online medical records. The model included the interaction of ADI quintiles and racioethnicity with covariates: internet access, age, gender, metropolitan status, general health status, health insurance, and education. We plotted the predicted probabilities of the interaction of ADI quintiles and racioethnicity (Figure 1). The 95% confidence intervals of each interaction are displayed on the plot.
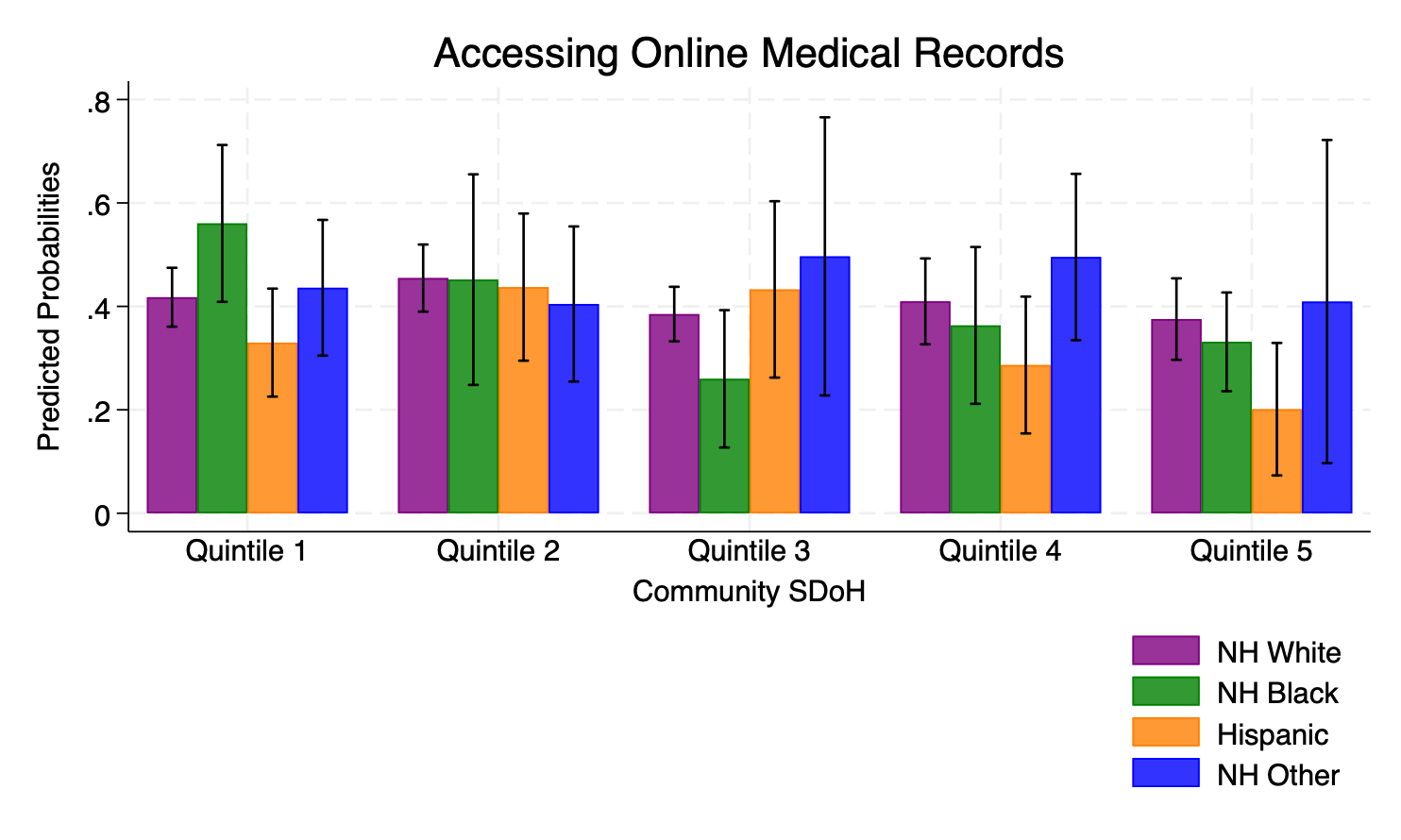
Figure 2.Relative Proportions of Individuals from Specific Racioethnic Populations who use Online Medical Records by ADI Quintile and Internet Source
NOTE: Chi-square tests were used to assess if there are associations between racioethnicity, community SDoH, and internet sources for those who access their online medical record. There was a difference for home, work, and mobile device in distributions across quintiles and racioethnicity with p-values < 0.05. ADI: Area Deprivation Index; NH: Non-Hispanic; Q1: Quintile 1 (ADI rank of 1-20); Q2: Quintile 2 (ADI rank of 21-39); Q3: Quintile 3 (ADI rank of 40-59); Q4: Quintile 4 (ADI rank of 60-80); Q5: Quintile 5 (ADI rank of 81-100).
Post hoc Analysis
We plotted the weighted population estimates of Internet sources by racioethnicity and ADI quintiles for those who accessed online medical records (Figure 2). For Internet sources, we used the HINTS question, “How often do you access the Internet through each of the following? a. Computer at home b. Computer at work c. Computer in a public place (library, community center, other) d. On a mobile device (cell phone/smart phone/tablet).” Answer options for each sub question were “Daily,” “Sometimes,” “Never,” and “Not Applicable.” For each Internet source, “Daily” and “Sometimes” were recoded to “Yes,” and “Never” was recoded to “No.”
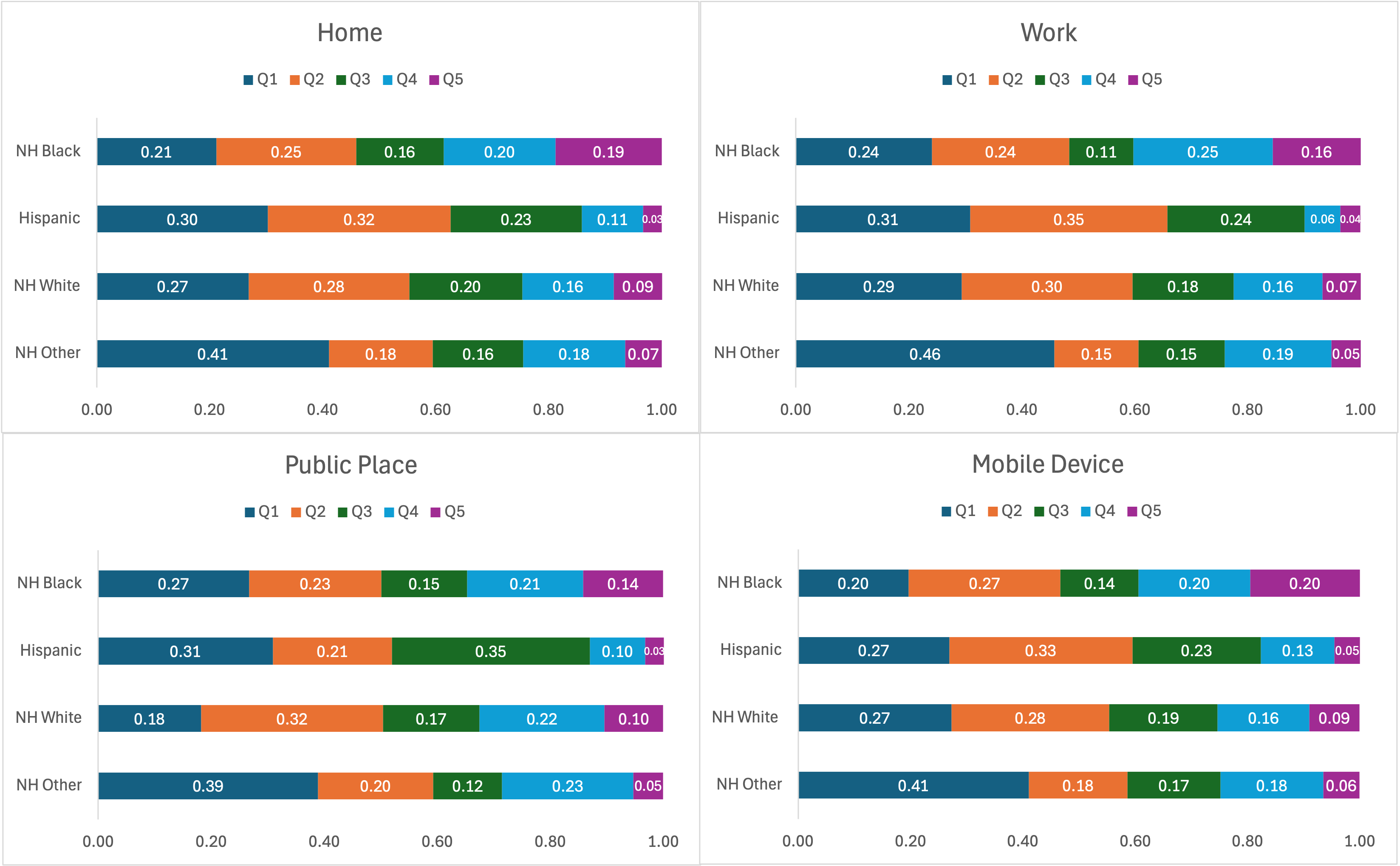
Figure 1.Predicted Probabilities of Access to Online Medical Record by ADI Quintile and Racioethnicity
NOTE: Predicted probabilities are based on population weight estimates (n = 4,211; N = 316,165,858). Error bars are 95% confidence intervals of each interaction. SDoH: Social Determinants of Health; ADI: Area Deprivation Index; NH: Non-Hispanic; Q1: Quintile 1 (ADI rank of 1-20); Q2: Quintile 2 (ADI rank of 21-39); Q3: Quintile 3 (ADI rank of 40-59); Q4: Quintile 4 (ADI rank of 60-80); Q5: Quintile 5 (ADI rank of 81-100).
We also obtained estimates for our main predictors using a two-stage model to predict the likelihood of online medical record use and intensity of online medical record use based on a weighted zero-inflated order logistic regression model.28 We categorized the outcome variable into three groups: “None,” “1 to 5 times,” and “6 or more times” to explore the differences between nonusers, users that access the online medical record at least bi-monthly, and those that access it less frequently over a 12-month period. We calculated predicted probabilities for each group (results not shown) and found similar results to our primary analysis. Stata/ME version 18.0 was used to conduct all analyses.
RESULTS
A combined analytical dataset was created with 16,092 pooled observations from all four HINTS 5 cycles (3285 [20.41%] from Cycle 1, 2017; 3504 [21.77%] from Cycle 2, 2018; 5438 [33.79%] from Cycle 3, 2019; 3865 [24.02%] from Cycle 4, 2020). There were 14,103 respondents who answered if they accessed their online medical record, and 5,766 (40.8%) responded that they had.
Figure 1 shows the predicted probabilities of accessing the online medical record by each ADI quintile and racioethnicity. Predicted probabilities for accessing online medical records were lowest in ADI quintile 5 for NH White and Hispanic communities. Predicted probabilities were highest in ADI quintiles 1 and 2 for NH White, NH Black, and Hispanic communities. Predicted probabilities were similar across all ADI quintiles for NH White communities. NH White communities were more likely to access the online medical record than NH Black for all ADI quintiles except for ADI quintile 1. NH White communities had a higher predicted probability of accessing online medical records compared to NH Black and Hispanic communities for the higher ADI quintiles (more deprivation).
Figure 2 displays the relative proportions of individuals from specific racioethnic populations who use online medical records by ADI quintile and Internet source. Among each racioethnic community, NH Black, Hispanic, and NH Other communities had a relatively higher proportion of respondents who accessed the Internet from a public place than NH White communities in ADI quintile 1. NH Black communities reported the highest use of all four Internet sources across the higher ADI quintiles (more deprivation) among all racioethnic communities. Among respondents who identified as Hispanic, those who lived in higher ADI quintiles accessed the Internet the least, across all racioethnic communities and Internet sources.
Our zero-inflated ordinal logistic regression analysis indicated lower probabilities of higher intensity online medical record use among all racioethnic communities. The range of predicted probabilities (between 0 and 1) for reporting no access to online medical records was 0.48 to 0.80. For accessing the online medical record 1 to 5 times, the range of predicted probabilities was 0.18 to 0.39. Predicted probabilities for accessing the online medical record 6 or more times were between 0.02 and 0.14. NH Black and Hispanic communities had higher predicted probabilities of not accessing the online medical record than NH White communities in higher ADI quintiles. In the models predicting access to the online medical record 1 to 5 times and 6 or more times, NH White communities were more likely to access the online medical record than NH Black and Hispanic communities in higher ADI quintiles.
DISCUSSION
Principal findings
In this brief report, our primary analysis demonstrated differences in the predicted probabilities for accessing online medical records associated with the intersectionality of racioethnicity and cSDoH. There was a variation in Internet sources accessed by racioethnicity and cSDoH among those who accessed online medical records (Figure 2), with higher use in some ADI quintiles for specific racioethnic communities. These results illustrate a complex interplay between the influences of racioethnicity, cSDoH, digital inclusion, and online medical record access and use. Our results align with previous studies in which NH Black and Hispanic communities were found to be less likely to access their online medical record compared to NH White communities in more disinvested communities.11,23,29,30 Among online medical record users, NH Black communities accessed the Internet the most, and Hispanic communities accessed the Internet the least in higher ADI quintiles across all racioethnic communities and Internet sources. Differences in Internet sources, racioethnicity, and communities support other studies highlighting potential contributors to the digital divide.31,32
It is important to consider the intersection between racioethnicity and cSDoH to promote health equity.33 Policy initiatives should prioritize addressing racial disparities in the most disinvested communities to reduce health inequities across the US.33,34 Policymakers can use cSDoH such as ADI to help make well-informed decisions on allocating resources and implementing interventions that can improve healthcare access.33,35 The Center for Medicare and Medicaid Services has used ADI in their policy updates on payment and care models to promote health equity.36 Similar approaches may be useful for reimbursement models, with the additional incorporation of factors such as intersectionality and digital inclusion to augment health equity initiatives. Additionally, community partners can also contribute to digital health equity initiatives by providing resources like technology-related support groups to communities in need.37
Implications for Practice
Healthcare institutions can prioritize tailored strategies that consider the community’s availability of devices and Internet access to encourage individuals to engage with digital health tools.10,17 Care team members within these healthcare institutions must be aware of the effects of the intersection of non-medical factors (e.g., racioethnicity) and community characteristics on patient care.38 It is important to consider Internet accessibility, digital affordability, and digital literacy39 for those with limited access to their online medical records. For example, social workers can advocate for patients living in marginalized communities and ensure that they can access digital resources, reducing the digital divide.39 In addition to practitioners, health information professionals could evaluate the adoption of online medical records and their use to encourage digital health equity using an intersectional perspective.40,41 An area-dependent measure such as ADI can be used to identify communities that may need tailored interventions (e.g., community events and campaigns) to promote online medical record use and education to manage overall health.42 Health information professionals should incorporate cultural competency tools and skills to promote digital equity in disinvested communities.43 Health information professionals can become more aware of digital inclusion and equity by attending training programs44,45 focused on intersectionality, which can help motivate and build trust between patients and health systems.
Limitations
There are some limitations to our study. First, we cannot infer causality since HINTS uses a cross-sectional design. Second, HINTS provides survey data that can be susceptible to recall bias. However, HINTS utilizes sampling and survey weights to mitigate potential biases and increase generalizability.46 ADI may not have included all relevant cSDoH variables related to our dependent variable: access and use of online medical records. Lastly, ADI may not fully capture socioeconomic characteristics since it was created based on census blocks.47
CONCLUSIONS
We used a nationally representative sample by leveraging HINTS data to explore the effects of racioethnicity, cSDoH, and Internet sources on access to online medical records. We found variations in predicted probabilities for accessing the online medical record and variations in relative weighted proportions for accessing the Internet from different sources across ADI quintiles and specific racioethnic communities. Further investigation can help policymakers design targeted health interventions and implement strategies to promote digital health equity.
Disclosures
The authors have nothing to disclose.
Funding
The authors received no funding for this research.
Data Availability
The data used for this study were obtained from the National Cancer Institute’s (NCI) Health Information National Trends Survey. The main data set is publicly available for access at https://hints.cancer.gov/. NCI provided the restricted geocoded data used in our study.
Bibliography
-
1.
Richardson LJ, Brown TH. (En)Gendering Racial Disparities in Health Trajectories: A Life Course and Intersectional Analysis.
SSM - Population Health. 2016;2:425-435. doi:
10.1016/j.ssmph.2016.04.011. PMID:28111630
-
2.
Magesh S, Daniel J, Wei TL, et al. Disparities in COVID-19 Outcomes by Race, Ethnicity, and Socioeconomic Status: A Systematic-Review and Meta-analysis.
JAMA network open. 2021;4(11):e2134147. doi:
10.1001/jamanetworkopen.2021.34147. PMID:34762110
-
3.
Babu S, Ganguly P, Shettigar N, Lin CH. Impact of Social Determinants of Health on Outcomes for Patients with Adult Congenital Heart Disease.
Current cardiology reports. 2024;26(6):539-544. doi:
10.1007/s11886-024-02059-w
-
4.
Zhang Y, Li J, Yu J, Braun RT, Casalino LP. Social Determinants of Health and Geographic Variation in Medicare per Beneficiary Spending.
JAMA network open. 2021;4(6):e2113212. doi:
10.1001/jamanetworkopen.2021.13212. PMID:34110394
-
5.
Emidio OM, Cutrona SL, Person SD, Mazor KM, Frisard C, Lemon SC. Association of Neighborhood-Level Social Determinants of Health with Psychosocial Distress in Patients Newly Diagnosed with Lung Cancer.
Cancer Reports (Hoboken, NJ). Published online 2022:e1734. doi:
10.1002/cnr2.1734. PMID:36250328
-
-
7.
Bowleg L. Evolving Intersectionality Within Public Health: From Analysis to Action.
American journal of public health. 2021;111(1):88-90. doi:
10.2105/AJPH.2020.306031. PMID:33326269
-
8.
Alvidrez J, Greenwood GL, Johnson TL, Parker KL. Intersectionality in Public Health Research: A View From the National Institutes of Health.
American journal of public health. 2021;111(1):95-97. doi:
10.2105/AJPH.2020.305986. PMID:33326274
-
9.
Bear Don’t Walk J, Bear Don’t Walk OJ, Paullada A, et al. Opportunities for Incorporating Intersectionality into Biomedical Informatics.
Journal of Biomedical Informatics. Published online 2024:104653. doi:
10.1016/j.jbi.2024.104653. PMID:38734158
-
-
11.
Walker DM, Hefner JL, Fareed N, Huerta TR, McAlearney AS. Exploring the digital divide: age and race disparities in use of an inpatient portal. Telemed J E Health. 2020;26(5):603-613.
-
-
13.
Wang ML, Gago CM, Rodriguez K. Digital Redlining-The Invisible Structural Determinant of Health.
The Journal of the American Medical Association. 2024;331(15):1267-1268. doi:
10.1001/jama.2024.1628
-
14.
McCall T, Asuzu K, Oladele CR, Leung TI, Wang KH. A Socio-Ecological Approach to Addressing Digital Redlining in the United States: A Call to Action for Health Equity.
Frontiers in digital health. 2022;4(897250). doi:
10.3389/fdgth.2022.897250. PMID:35924138
-
15.
Sieck CJ, Sheon A, Ancker JS, Castek J, Callahan B, Siefer A. Digital Inclusion as a Social Determinant of Health.
Npj Digital Medicine. 2021;4(1):52. doi:
10.1038/s41746-021-00413-8. PMID:33731887
-
16.
Lyles CR, Wachter RM, Sarkar U. Focusing on Digital Health Equity.
JAMA. 2021;326(18):1795-1796. doi:
10.1001/jama.2021.18459
-
-
18.
Hogg-Graham R, Scott AM, Clear ER, Riley EN, Waters TM. Technology, Data, People, and Partnerships in Addressing Unmet Social Needs within Medicaid Managed Care.
BMC Health Services Research. 2024;24(1):368. doi:
10.1186/s12913-024-10705-w. PMID:38521923
-
19.
Cartier Y, Fichtenberg C, Gottlieb LM. Implementing Community Resource Referral Technology: Facilitators and Barriers Described by Early Adopters.
Health Affairs (Project Hope). 2020;39(4):662-669. doi:
10.1377/hlthaff.2019.01588
-
20.
Yamin CK, Emani S, Williams DH, et al. The Digital Divide in Adoption and Use of a Personal Health Record.
Archives of Internal Medicine. 2011;171(6):568-574. doi:
10.1001/archinternmed.2011.34
-
21.
Chamberlain AM, St Sauver JL, Finney Rutten LJ, et al. Associations of Neighborhood Socioeconomic Disadvantage With Chronic Conditions by Age, Sex, Race, and Ethnicity in a Population-Based Cohort.
Mayo Clinic Proceedings. 2022;97(1):57-67. doi:
10.1016/j.mayocp.2021.09.006. PMID:34996566
-
22.
Daniels B, McGinnis C, Topaz LS, et al. Bridging the digital health divide-patient experiences with mobile integrated health and facilitated telehealth by community-level indicators of health disparity.
Journal of the American Medical Informatics Association: JAMIA. 2024;31(4):875-883. doi:
10.1093/jamia/ocae007. PMID:38269583
-
23.
Lorence DP, Park H, Fox S. Racial Disparities in Health Information Access: Resilience of the Digital Divide.
Journal of Medical Systems. 2006;30(4):241-249. doi:
10.1007/s10916-005-9003-y
-
-
-
26.
Swoboda CM, DePuccio MJ, Fareed N, McAlearney AS, Walker DM. Patient Portals: Useful for Whom and for What? A Cross-Sectional Analysis of National Survey Data. Appl Clin Inform. 2021;12(3):573-581.
-
27.
Singh S, Polavarapu M, Arsene C. Changes in Patient Portal Adoption Due to the Emergence of COVID-19 Pandemic.
Informatics for Health & Social Care. 2023;48(2):125-138. doi:
10.1080/17538157.2022.2070069
-
-
29.
Yoon H, Jang Y, Vaughan PW, Garcia M. Older Adults’ Internet Use for Health Information: Digital Divide by Race/Ethnicity and Socioeconomic Status.
Journal of Applied Gerontology: The Official Journal of the Southern Gerontological Society. 2020;39(1):105-110. doi:
10.1177/0733464818770772
-
30.
Wang H, Manning SE, Ho AF, Sambamoorthi U. Factors Associated with Reducing Disparities in Electronic Personal Heath Records Use Among Non-Hispanic White and Hispanic Adults.
Journal of Racial and Ethnic Health Disparities. Published online 2022. doi:
10.1007/s40615-022-01307-5
-
31.
Li Y, Turner-Lee N, Gambhir S, Baek M. Does Place Really Matter? Broadband Availability, Race and Income. Joint Center for Political and Economic Studies Working Paper Series. Published online 2011.
-
32.
Ray R, Sewell AA, Gilbert KL, Roberts JD. Missed Opportunity? Leveraging Mobile Technology to Reduce Racial Health Disparities.
Journal of Health Politics, Policy and Law. 2017;42(5):901-924. doi:
10.1215/03616878-3940477
-
-
34.
Williams DR, Jackson PB. Social Sources of Racial Disparities in Health.
Health Affairs (Project Hope). 2005;24(2):325-334. doi:
10.1377/hlthaff.24.2.325
-
35.
Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible: The Neighborhood Atlas.
The New England Journal of Medicine. 2018;378(26):2456-2458. doi:
10.1056/NEJMp1802313. PMID:29949490
-
36.
Morenz AM, Liao JM, Au DH, Hayes SA. Area-Level Socioeconomic Disadvantage and Health Care Spending: A Systematic Review.
JAMA network open. 2024;7(2):e2356121. doi:
10.1001/jamanetworkopen.2023.56121. PMID:38358740
-
37.
Richardson S, Lawrence K, Schoenthaler AM, Mann D. A Framework for Digital Health Equity.
Npj Digital Medicine. 2022;5(1):119. doi:
10.1038/s41746-022-00663-0. PMID:35982146
-
38.
Jonnalagadda P, Swoboda CM, Fareed N. Using area-level measures of social determinants of health to deliver improved and effective health care.
Journal of Hospital Management and Health Policy. Published online December 25, 2020:4. doi:
10.21037/jhmhp-20-100
-
39.
Sanders CK, Scanlon E. The Digital Divide Is a Human Rights Issue: Advancing Social Inclusion Through Social Work Advocacy.
Journal of human rights and social work. 2021;6(2):130-143. doi:
10.1007/s41134-020-00147-9. PMID:33758780
-
40.
Tapuria A, Porat T, Kalra D, Dsouza G, Xiaohui S, Curcin V. Impact of patient access to their electronic health record: systematic review.
Informatics for health & social care. 2021;46(2):192-204. doi:
10.1080/17538157.2021.1879810
-
-
42.
Dow D. Mapping Health Disparities: Leveraging Area-Based Deprivation Indices for Targeted Chronic Disease Intervention.
Delaware journal of public health. 2024;10(1):106-110. doi:
10.32481/djph.2024.03.14. PMID:38572137
-
43.
McGregor B, Belton A, Henry TL, Wrenn G, Holden KB. Improving Behavioral Health Equity through Cultural Competence Training of Health Care Providers.
Ethnicity & disease. 2019;29(Suppl 2):359-364. doi:
10.18865/ed.29.S2.359. PMID:31308606
-
44.
Chohan SR, Hu G. Strengthening Digital Inclusion through E-Government: Cohesive ICT Training Programs to Intensify Digital Competency.
Information Technology for Development. 2020;28(1):16-38. doi:
10.1080/02681102.2020.1841713
-
45.
Longhini J, Rossettini G, Palese A. Digital Health Competencies Among Health Care Professionals: Systematic Review.
Journal of medical Internet research. 2022;24(8):e36414. doi:
10.2196/36414. PMID:35980735
-
46.
Elkefi S, Yu Z, Asan O. Online Medical Record Nonuse among Patients: Data Analysis Study of the 2019 Health Information National Trends Survey.
Journal of Medical Internet Research. 2021;23(2):e24767. doi:
10.2196/24767. PMID:33616539
-
47.
Sprowls GR, Layton BO, Carroll JM, Welch GE, Kissenberth MJ, Pill SG. Neighborhood Socioeconomic Disadvantages Influence Outcomes Following Rotator Cuff Repair in the Non-Medicaid Population.
Journal of Shoulder and Elbow Surgery. Published online 2024. doi:
10.1016/j.jse.2024.03.002