Download PDF
CE Quiz
Abstract
Incorporating experiential learning in health information (HI) is essential to prepare students for the rapidly evolving healthcare landscape, where practical skills and real-world application are critical for success. This manuscript explores the integration of experiential learning into HI education, highlighting the importance of bridging theoretical knowledge with real-world application. By incorporating diverse learning methods—such as internships, simulations, project-based learning, role-playing exercises, and practicums—HI programs can enhance students’ technical proficiency, strengthen their critical thinking and communication skills, and deepen their understanding of healthcare systems. This paper demonstrates how each experiential learning approach aligns with HI competencies, particularly in areas such as data management, privacy protection, and healthcare compliance. These methods contribute directly to the development of essential skills, preparing students to navigate and address the complex challenges of modern healthcare environments. In addition to outlining the benefits of these methods, the manuscript addresses implementation challenges, including resource limitations and the need for industry partnerships. Recommendations are provided to help HI educators effectively integrate experiential learning into curricula, ensuring students gain hands-on experience that prepares them for the evolving demands of the healthcare workforce.
Introduction
Health information (HI) plays a vital role in the healthcare environment by ensuring the systematic management, safeguarding, and integrity of patient data. While the importance of collecting and organizing healthcare information had long been recognized, the profession of HI formally originated in 1928 with the formation of the Association of Record Librarians of North America (ARLNA),1 later evolving into the American Health Information Management Association (AHIMA). This organization was instrumental in shaping HI education and setting industry standards, which laid the foundation for current HI curricula.
Over time, HI educational programs have expanded to cover critical areas such as medical coding, information governance, data analytics, privacy, security, and technology—each essential for maintaining accurate and secure health information systems.2 As healthcare systems become increasingly complex and interconnected, HI professionals must combine technical expertise with essential soft skills, including critical thinking, decision making, and communication. In response to these demands, HI education has integrated hands-on, real-world learning experiences to better prepare students for the challenges of an evolving healthcare landscape.3
Today, HI education faces several challenges, including the rapid advancement of technology and the increasing integration of digital health technologies like Electronic Health Records (EHRs), telemedicine, and health information exchanges.4 The rising demand for data analytics and cybersecurity expertise, along with the need for professionals skilled in both technical and managerial roles, requires HI programs to continuously evolve.5 A significant challenge is the rise of artificial intelligence (AI) tools, which now perform tasks previously reliant on human input, such as answering multiple-choice questions or analyzing large datasets. This shift has prompted a reevaluation of the effectiveness of traditional assessment methods in evaluating critical thinking and problem-solving skills, since AI platforms can often answer these rote questions.
Additionally, HI educators must navigate resource limitations, varying levels of industry collaboration, and the need for more interprofessional education opportunities that reflect the collaborative nature of healthcare teams. Emerging trends in HI education emphasize the integration of experiential learning, which not only enhances students’ technical skills but also prepares them to solve real-world problems, adapt to rapidly changing technologies, and collaborate across healthcare settings. To meet these demands, educators are exploring innovative assessment methods and teaching approaches that foster creativity, collaboration, and deeper understanding—skills that AI cannot easily replicate.
This growing need for adaptable, skilled professionals highlights the importance of incorporating experiential learning into HI education, enabling students to gain the hands-on experience essential for navigating the complexities of the modern healthcare environment.
Manuscript Objective and Scope
In this manuscript, we discuss the integration of experiential learning into HI education and its role in enhancing student preparedness for the workforce. We also outline various experiential learning modalities—including internships, simulations, project-based learning, role-playing, and educational site visits—and how these methods align with HI competencies. Additionally, we highlight how these learning strategies contribute to the development of essential skills such as data management, privacy protection, and healthcare compliance.
We also aim to describe the benefits of incorporating experiential learning into HI curricula, focusing on the enhancement of critical thinking, communication, and technical proficiency. Acknowledging the challenges of implementing these strategies—such as resource constraints and time limitations—we propose practical solutions for overcoming these obstacles. Ultimately, our goal in writing this article is to provide HI educators with actionable guidance on embedding experiential learning into their programs, ensuring that students acquire the hands-on experience needed to succeed in the healthcare workforce.
Need for Experiential Learning
Experiential learning is a crucial component of HI education, enabling students to bridge the gap between theoretical knowledge and its practical application in the workplace.6,7 Kolb’s Experiential Learning Theory8 outlines this process as a cycle in which students engage with real-world experiences, reflect on them, and apply the insights gained to future situations. Through experiential learning methods such as role-playing, internships, simulations, and project-based learning, HI students can engage directly with the technologies and processes they will encounter in their careers.
As healthcare systems become more complex and technology-driven, HI professionals must develop practical, tech-oriented skills that extend beyond traditional classroom learning. Experiential learning allows HI students to interact with cutting-edge technologies such as AI, machine learning, predictive analytics, and EHR optimization—tools that are increasingly transforming healthcare practices.9 By engaging with these tools in real-world settings, students can develop essential technical skills to address data management, privacy compliance, and the growing role of technology in healthcare decision making. This hands-on experience ensures that students are well-equipped to navigate emerging challenges in the healthcare sector.3
Incorporating experiential learning into HI education not only allows students to refine their technical skills but also emphasizes the development of crucial soft skills. These include problem-solving, critical thinking, and collaboration—skills that are essential for HI professionals to adapt to the fast-evolving healthcare landscape.10 By engaging in practical activities, students cultivate these competencies, enabling them to work effectively within interdisciplinary teams, make informed decisions, and solve complex problems.11 These soft skills, coupled with technical expertise, ensure that HI professionals are prepared to meet the demands and challenges of modern healthcare environments.
This shift toward integrating both technical and soft skills through experiential learning is grounded in established learning theories, particularly Kolb’s Experiential Learning Theory8–which again, provides a framework for understanding how students learn from hands-on experiences. The next section will explore this theory in detail, examining how it supports the design and implementation of effective experiential learning strategies in HI education.
Theoretical Foundations of Experiential Learning
Experiential learning is a process through which individuals learn by directly engaging in an experience, reflecting on that experience, and applying the insights gained to future situations.12 This concept was formalized by psychologist and education theorist David Kolb, who posited that experience is the foundation of learning and development. Kolb defined learning as “the process whereby knowledge is created through the transformation of experience.”8 The theory is rooted in the work of several influential scholars, including Piaget, Dewey, Lewin, and Vygotsky, whose contributions shaped its development.13
Kolb’s experiential learning theory outlined four distinct learning styles: diverging (feeling and watching), assimilating (thinking and watching), converging (thinking and doing), and accommodating (feeling and doing).14 According to Kolb, learners process information in two dimensions: by comprehending or grasping information, and by transforming or processing that information through experiences.15
Components of the Experiential Learning Cycle
Kolb suggested that effective learning occurs as individuals move through a cyclical process composed of four key components: concrete experience (CE), reflective observation (RO), abstract conceptualization (AC), and active experimentation (AE).13,14,16 Figure 1 illustrates these components.14
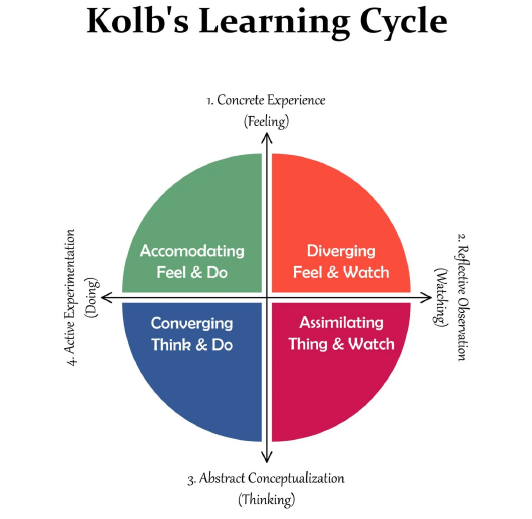
Figure 1.Kolb’s Learning Cycle
Figure 1. Kolb’s Learning Cycle. Reprinted with permission from Shutterstock.
- Concrete Experience (CE): This stage involves engaging in new experiences or reexamining existing ones through direct interaction or hands-on activities.14,16 In HI education, this could involve simulations in which students manage patient data in an EHR system or handling real-world healthcare data during an internship. These experiences help HI students apply theoretical concepts, such as data entry or privacy protocols, in real-world contexts.
-
Reflective Observation (RO): At this stage, students reflect on their experiences, comparing them with prior knowledge and identifying differences or areas of improvement.14,16 For HI students, this may occur after completing a simulation or project where they reflect on their actions, such as troubleshooting a data security breach or handling a data privacy concern. The reflection process allows students to recognize how their actions align with industry standards or areas where improvement is needed.
-
Abstract Conceptualization (AC): Based on their reflections, students develop new ideas or modify existing concepts during the Abstract Conceptualization phase.14,16 In HI, this could involve revising approaches to data governance after analyzing an EHR implementation. For instance, an HI student might conceptualize a more efficient workflow for data entry after reflecting on how their previous attempts could be improved. This phase is crucial for linking hands-on experience with broader theories of healthcare information management.
-
Active Experimentation (AE): In this phase, students apply the revised concepts in a real-world context to test their validity.14,16 For HI students, this might mean applying newly learned data management practices during their next internship or experimenting with an updated security protocol in a healthcare environment. The aim is to refine skills, test new ideas, and solve real-world problems, such as ensuring compliance with updated healthcare regulations or improving patient data accuracy.
These four stages of the experiential learning cycle—CE, RO, AC, and AE—are integral to developing both the technical and soft skills necessary for success in HI education. Grounded in Kolb’s theory, these experiential learning methods help students develop key competencies that better equip them to navigate the complexities of the evolving healthcare landscape and workforce.
Experiential learning, though not a new concept in medical education, has gained increasing prominence over the past two decades in public health and healthcare management programs.13 This shift reflects the recognized benefits of experiential learning in equipping students with the skills necessary to process and apply information in real-world contexts, both inside and outside the classroom, preparing them for practice in an ever-evolving field.17,18 Experiential learning activities—such as role-playing, where students simulate professional scenarios to enhance communication and decision making; internships, which provide hands-on experience in real-world healthcare settings; problem-solving exercises, where students apply critical thinking to resolve complex issues; problem-based learning, focusing on collaborative solutions to practical, real-world problems; and simulations, where students engage in virtual or physical healthcare scenarios—provide students with opportunities to engage in meaningful, hands-on experiences.3
Table 1 outlines these experiential learning activities, designed with careful consideration of key educational objectives. It provides a breakdown of each activity by description, subject areas, education level, estimated time commitment, location format (in-person, hybrid, or online), instructional effort, and strategies for assessment and skills measurement. These elements ensure that each activity is aligned with professional competencies, fostering the development of practical, career-ready skills. By engaging in these activities, students actively practice key skills and behaviors, reflecting on their experiences and refining their abilities through iterative learning and adjustment.19
Table 1.Experiential Learning Activities
| Role Playing |
Subject Areas |
Level |
Estimated Time Commitment |
Format |
Instructional Effort |
Support Type |
Assessment Format |
Skills Measured |
| Students will practice gathering and refining healthcare data requests for a data warehouse system using an AI language model (LLM) or collaborating with a classmate, alternating between acting as a data requestor or a data analyst. They will engage in a structured discussion to determine necessary data variables for a patient report. |
Clinical Data Management; Informatics, Analytics, and Data Use |
Associate, Baccalaureate |
1-2 hours: 30-45 minutes for role playing and discussion; 30 minutes for written summary, reflection, and final submission. |
In person, hybrid, or online |
Minimal: The instructor might provide guidance on best practices. |
Instructor required for debrief with Q&A |
Written reflection; evaluation based on student's ability to connect activity to best practices, articulate learning, and express different perspectives. |
Communication, decision making, teamwork |
| Internship |
Subject Areas |
Level |
Estimated Time Commitment |
Format |
Instructional Effort |
Support Type |
Assessment Format |
Skills Measured |
| Third- or fourth-year undergraduate students will create a health information-related report (e.g., discharge summary turnaround, bed utilization, or provider delinquent report) with the guidance of a health information professional. Using healthcare data management software, students will refine and present their findings to relevant stakeholders. |
Data Structure, Content, and Information Governance |
Baccalaureate |
3-5 hours: data collection, report generation. 1-2 hours presentation preparation. 1-3 hours self- reflection and final submission. |
In person, hybrid, or online |
Moderate to High: Scheduling and collaboration with HI professional. |
Required HI professional |
Quality of report (e.g., thoroughness, accuracy, clarity). Stakeholder presentation: Rubric with instructor feedback. Reflection: Self-reflection essay. |
Decision making, communication, teamwork, and problem solving |
| Problem-Solving Exercise |
Subject Areas |
Level |
Estimated Time Commitment |
Format |
Instructional Effort |
Support Type |
Assessment Format |
Skills Measured |
| Students will collaborate in multi-disciplinary teams to investigate a real-world decline in Case-Mix Index (CMI) at a rural acute care hospital. Using their HI knowledge, they will analyze potential contributing factors, propose an investigative plan, and reflect on their teamwork experience. This activity applies data analytics, informatics, and revenue cycle management concepts to hospital operations. |
Revenue Cycle Management |
Associate, Baccalaureate, Master’s |
2-3 hours: identifying factors and creating a plan to improve those factors. 30 minutes teamwork reflection and final submission. |
In person, hybrid, or online |
Moderate to High: Guiding teams through the issues and investigative process. |
Independent activities by students |
Accuracy of problem identification.Thoroughness of investigative plan. Reflection: Teamwork reflection essay. |
Critical thinking, decision making, and analytical skills |
| Problem-Based Learning |
Subject Areas |
Level |
Estimated Time Commitment |
Format |
Instructional Effort |
Support Type |
Assessment Format |
Skills Measured |
| In this problem-based assignment, students will be introduced to HL7 Fast Healthcare Interoperability Resources (FHIR) and investigate how Health Level Seven International (HL7) organizes its work to specify and promote FHIR adoption. |
Informatics, Analytics, and Data Use |
Baccalaureate |
3-5 hours to review resources and conduct investigation ways in which FHIR can be adopted. 30 minutes assignment reflection and final submission. |
In person, hybrid, or online |
Minimal: Self-paced modules for independent learning. |
Independent activities by students |
Reflection: Connection to FHIR resources and clarity of explanation. |
Leadership, problem solving, and critical thinking |
| Simulation |
Subject Areas |
Level |
Estimated Time Commitment |
Format |
Instructional Effort |
Support Type |
Assessment Format |
Skills Measured |
| This simulation exercise focuses on the implementation of a wound care application in a nursing workflow. Nursing and HI students collaborate in teams to use the application for real-time wound assessment and documentation. |
Informatics, Analytics, and Data Use |
Baccalaureate, Master's |
3-5 hours to implement a digital wound care application within an EHR system and collaborate with nursing students on wound assessment and documentation. |
In person |
Moderate to High: Significant coordination between nursing and HI students. Scheduling for simulation lab. Technical staff and faculty will need to support the student with the application. |
Instructor could guide students in teams to use the app for real-time wound assessment and documentation. Debrief with Q&A. |
Reflection: Connection to FHIR resources and clarity of explanation. |
Leadership, problem solving, and critical thinking |
Also, through experiential learning, health information education programs can ensure that their curricula remain relevant, equipping students with the practical skills and knowledge needed to transition seamlessly into the workforce.18 Furthermore, embedding core competencies and professional standards into authentic assessments throughout the curriculum supports the development of the knowledge, skills, and attitudes essential to the health information profession. This approach to pedagogy challenges educators to critically assess their learning activities, fostering the creation of more effective and authentic opportunities for student learning. The following section provides a detailed discussion of a simulation example, illustrating how these principles can be applied in practice.
One practical application of experiential learning theories is interdisciplinary simulation.20,21 Simulation provides HI students with the opportunity to apply their knowledge in real-world scenarios, working collaboratively with other healthcare professionals. Below is an example of a simulation that successfully integrates HI competencies with nursing practice, demonstrating the value of experiential learning in preparing students for professional roles.
Simulation Overview
In this example, HI and nursing students collaborate in a simulation lab to implement a digital wound care application within an EHR system. The goal is for students to engage in an interprofessional education (IPE) experience that allows them to develop their technological proficiency, and collaborative practices in a realistic, controlled environment.
Learning Context
This simulation is designed for HI students enrolled in a Bachelor of Science in Health Information Management (BSHIM) program who are taking an “Electronic Health Record Systems & Digital Tools” course. The course covers EHR systems, data interoperability, clinical decision support tools, and digital healthcare technologies, which are essential to modern HI practice.
Alignment of Simulation Activity Phases with Kolb’s Learning Cycle
-
Orientation (15 minutes): HI students introduce the wound care application, demonstrating key features such as image capture, patient documentation, and record management. This phase helps HI students develop competencies in data management, privacy, and EHR system navigation.
CE: In this stage, students actively engage with the new technology, gaining hands-on experience that connects theoretical knowledge with practical application. Their direct interaction with the wound care application serves as the foundation for learning through action.
-
Application Practice (25 minutes): Nursing students perform real-time wound assessments using the application, while HI students provide hands-on guidance and technical support. HI students develop skills in troubleshooting, ensuring proper documentation, and supporting the seamless integration of technology with clinical workflows.
AE: During this phase, HI students apply the knowledge and skills they gained during the orientation by troubleshooting and assisting in real-time clinical settings. This hands-on practice allows them to experiment with solutions and adjust their approach based on immediate feedback and outcomes.
-
Debriefing (20 minutes): The group reflects on their experiences, discussing challenges faced, lessons learned, and opportunities for improving interdisciplinary collaboration and the use of technology in patient care. This phase fosters critical thinking and problem solving in real time, with HI students reflecting on their roles in supporting clinical decision making and data management.
RO, AC: In this stage, students reflect on their experiences during the simulation, considering what worked well and what could be improved. They analyze these reflections to develop new strategies or modify existing approaches, thereby enhancing their understanding of clinical and technical aspects of patient care and health information management.
Learning Objectives
-
Technical proficiency: Nursing students become proficient in using the wound care application, while HI students gain experience troubleshooting and assisting with digital tool integration.
-
Interdisciplinary collaboration: The simulation fosters teamwork between HI and nursing students, promoting communication and understanding of each profession’s role in patient care.
-
Critical thinking and problem solving: Both groups practice resolving issues related to technology and documentation in real time, enhancing their critical thinking skills.
-
Reflective practice: Post-simulation reflection allows students to analyze their performance and improve their skills for future scenarios.
Measuring Learning Outcomes
-
Technical proficiency: Assessed through image accuracy, upload functionality, and documentation precision, evaluated on a pass/fail basis.
-
HI student effectiveness: Evaluated using a rubric to assess HI students’ ability to support nursing students, with feedback collected from nursing students via satisfaction surveys.
-
Interprofessional communication: Measured through reflective essays and peer feedback, with active participation in debriefing sessions. Reflective practice activities help evaluate soft skills such as communication, critical thinking, and collaborative problem solving.
Discussion
Experiential learning has a critical role in HI education, contributing to students’ professional growth. Through avenues such as internships, simulations, and project-based activities, experiential learning offers HI students the chance to apply theoretical knowledge in real-world settings. This approach not only deepens their understanding but also equips them with essential skills for success in the rapidly evolving healthcare industry. For educators, experiential learning enhances student engagement and provides insightful feedback on how well the curriculum aligns with industry demands. It also ensures that emerging professionals are prepared to navigate the complexities of modern healthcare systems.
Despite its many advantages, integrating experiential learning into HI education comes with a range of challenges. Students often face barriers, such as limited access to quality internships or financial constraints, which may hinder their ability to gain meaningful, hands-on experience. Educators, in turn, may struggle with resource limitations, resistance to new teaching methods, and the need to make substantial adjustments to curricula. The healthcare industry also encounters challenges in establishing stable partnerships with educational institutions and ensuring adequate mentorship for students during experiential learning opportunities.
Several solutions are proposed to address these challenges. For students, virtual simulations, flexible internship scheduling, and financial support through scholarships or stipends can make experiential learning more accessible. Educators can benefit from building partnerships with healthcare organizations, incorporating guest speakers and virtual learning tools, and developing a flexible curriculum that seamlessly integrates hands-on experiences. Healthcare organizations can further contribute by fostering collaborative partnerships with HI programs, standardizing internship practices, and offering structured mentorship programs to guide students through their training.
Looking ahead, additional research is needed to assess the long-term impact of experiential learning on HI students’ career outcomes and to explore strategies for standardizing training across various healthcare institutions. Continued innovation in HI education is essential to ensure that future professionals possess the skills and knowledge necessary to thrive in an ever-evolving healthcare landscape.
Conclusions
Integrating experiential learning into HI education presents challenges, but the benefits for students, educators, and the healthcare industry are clear. By providing hands-on learning experiences that align with real-world applications, HI programs equip graduates with the technical and soft skills necessary to meet the dynamic needs of the healthcare sector. These experiences prepare students for immediate success in their careers while fostering long-term adaptability in a rapidly changing industry. Overcoming the obstacles faced by students, educators, and the healthcare industry requires collaboration, creativity, and innovation. The effort will be invaluable, ensuring a highly skilled HI workforce that is prepared to navigate the complexities of modern healthcare and drive future advancements in health information management.
Disclosures
The authors have nothing to disclose.
Funding
The authors received no funding for this research.
Submitted: March 11, 2025 EDT.
Accepted: May 16, 2025 EDT.
© American Health Information Management Association
Bibliography
-
1.
Gibson CJ, Dixon BE, Abrams K. Convergent evolution of health information management and health informatics: A perspective on the future of information professionals in health care.
Appl Clin Inform. 2015;6(1):163-184. doi:
10.4338/ACI-2014-09-RA-0077
-
-
3.
Tar Lim RB, Shin Chow DW, Zheng H. A scoping review of experiential learning in public health education from the perspective of students, faculty, and community partners.
J Exp Educ. Published online 2023. doi:
10.1177/10538259231171073
-
4.
Ritter BA, Gopalkrishnan SS, Sockbeson CES. The Next Generation of Pedagogy: Reflections from EdTech Leaders.
Journal of Management Education. 2024;48(4):610-633. doi:
10.1177/10525629231206182
-
-
6.
Branda D. Precepting HIM students: a multi-case study exploring the challenges of HIM hospital-based professional practice experience. Perspectives in Health Inf Manag. 2022;19(3).
-
7.
Phan N. Bridging the gap: A framework for experiential learning in higher education.
Bus Prof Commun Q. 2024;0(0):1-15. doi:
10.1177/23294906241292009
-
8.
Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. 2nd ed. Pearson Education, Inc; 2015.
-
9.
Ankem K, Uppala V, Durst A. Integrating experiential learning: Using an EHR system to teach CDSS in health informatics. Issues Inf Syst. 2019;20(3):1-10.
-
10.
Robinson K, Riley M, Prasad N, Nexhip A. Health information management students’ work-integrated learning (professional practice placement): Where do they go and what do they do?
Health Inf Manag J. Published online December 18, 2024. doi:
10.1177/18333583241303771
-
-
12.
Lewis LH, Williams CJ. Experiential Learning: A New Approach. Jossey-Bass; 1994:5-16.
-
13.
Kolb AY, Kolb DA. The Kolb Experiential Learning Profile, a Guide to Experiential Learning Theory, KELP Psychometrics and Research on Validity. Experience Based Learning Systems, LLC; 2021.
-
-
15.
Murrell PH, Claxton CS. Experiential learning theory as a guide for effective teaching.
Counselor Education and Supervision. 1987;27:4-14. doi:
10.1002/j.1556-6978.1987.tb00735.x
-
16.
Hall A. REAL Reflection Reflective Learning Communities: A Handbook for Facilitating Critical Reflection in the Classroom and Beyond. Virginia Commonwealth University; 2019.
-
17.
Chong SCS, Anderson K, Mackenzie-Stewart R, Hobbs C, Conna B. Embedding3 experiential learning in undergraduate health promotion curriculum.
Health Promot J Austral. 2022;33(S1):9-16. doi:
10.1002/hpja.629
-
18.
Cantor JA. Experiential Learning in Higher Education: Linking Classroom and Community. The George Washington University, Graduate School of Education and Human Development; 1995.
-
-
20.
Rossler K, Molloy MA, Pastva AM, Brown M, Xavier N. Healthcare simulation standards of best practiceTM simulation-enhanced interprofessional education.
Clinical Simulation in Nursing. 2021;58:49-53. doi:
10.1016/j.ecns.2021.08.01
-
21.
Ryan C, Johnson P, Mainey L, et al. These sims are different! Thematic analysis of interdisciplinary faculty experiences designing virtual simulations.
Clin Simul Nurs. 2025;98:1. doi:
10.1016/j.ecns.2024.101658